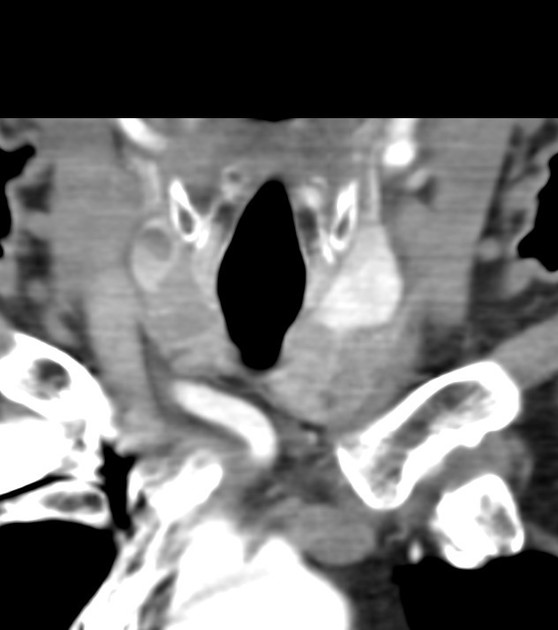
Thyroid nodules are any discrete lesion that can be delineated on imaging studies from the adjacent thyroid parenchyma. They can represent a range of benign or malignant conditions.
On this page:
Epidemiology
They are more common in females (4:1 F:M) and have an increasing prevalence with increasing age and reduced iodine intake 2,3. The incidence is estimated at 0.1% with a lifetime prevalence of 10% 3.
Clinical presentation
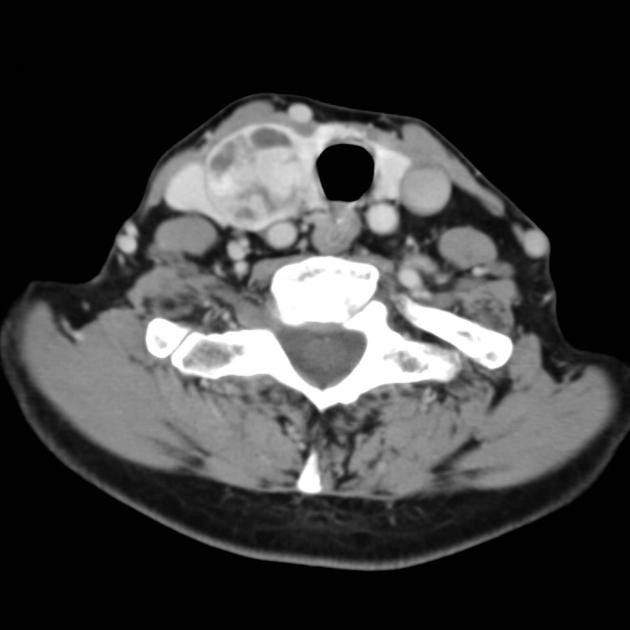
Thyroid nodules are a common incidental finding on imaging (see: incidental thyroid nodules), present in ~10% of CT and MRI neck examinations, ~50% (range 20-76%) of neck ultrasound, and 55% (range 50-65%) of autopsies 1-3. They can also be found on clinical examination as palpable lesions in the neck, although this clinical finding does not represent a thyroid nodule if there is no imaging correlate.
When symptomatic, patients may present with thyroid dysfunction or rarely compressive symptoms 3.
Pathology
Thyroid nodules are typically benign. The prevalence of malignancy (based on biopsy) in thyroid nodules is ~10% (range 4-6-15%) 3,4.
Aetiology
There are many causes of thyroid nodules, some of the more common causes are listed below:
-
benign nodules
-
follicular adenoma
thyroid cyst: simple, haemorrhagic
-
focal/asymmetrical thyroiditis
-
-
malignant nodules
Radiographic features
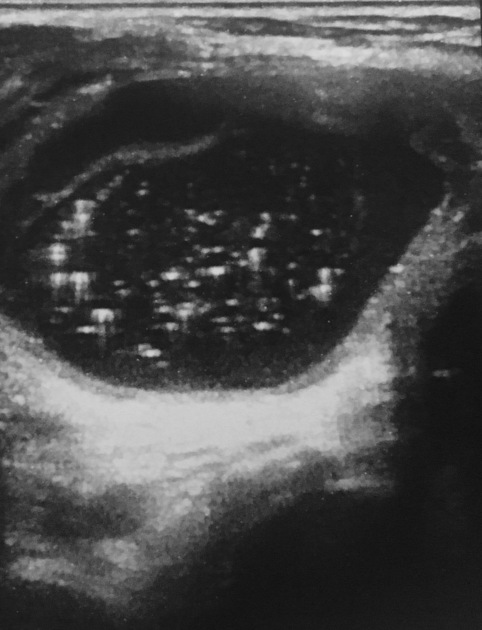
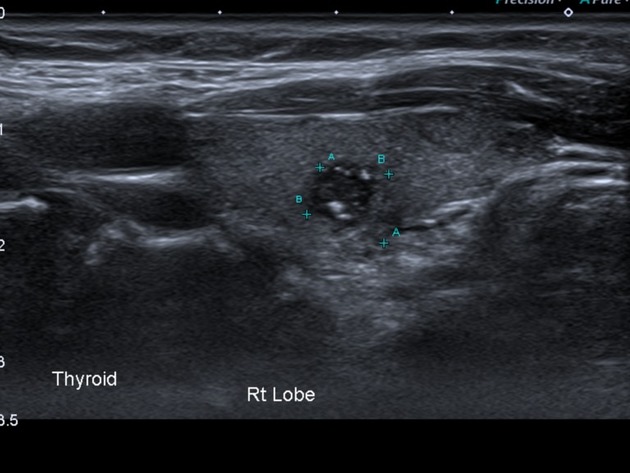
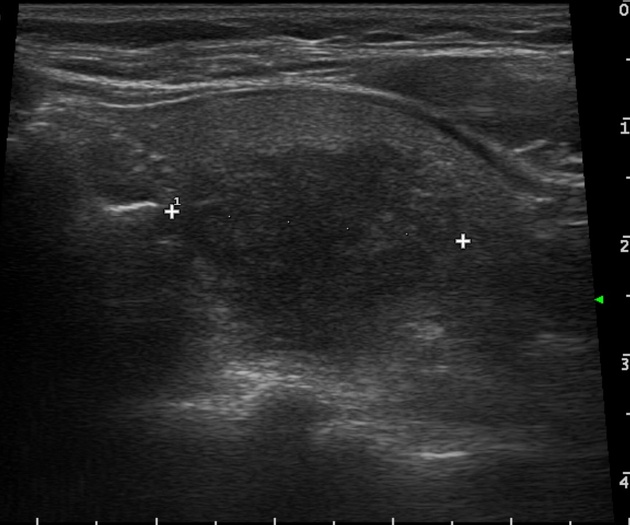
Ultrasound is the modality of choice for diagnostic assessment of thyroid nodules 4. It also allows for ultrasound-guided fine-needle aspiration of selected nodules.
Treatment and prognosis
Symptomatic benign thyroid nodules are commonly managed surgically (i.e. hemithyroidectomy/thyroidectomy 7). Thyroid nodule ablation is a less invasive alternative 7.
As thyroid nodules are commonly incidental, there are numerous classification systems to help with risk stratification. See article: Incidental thyroid nodules for further detail.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.