Twin-to-twin transfusion syndrome (TTTS), less commonly known as stuck twin syndrome, is a potential complication that can occur in a monochorionic twin pregnancy (either MCDA or MCMA).
On this page:
Epidemiology
This complication can occur in ~10% (range 15-25%) of monochorionic pregnancies, giving an estimated prevalence of ~1:2000 of all pregnancies.
Clinical presentation
Maternal abdominal distension has been described as a clinical feature.
Pathology
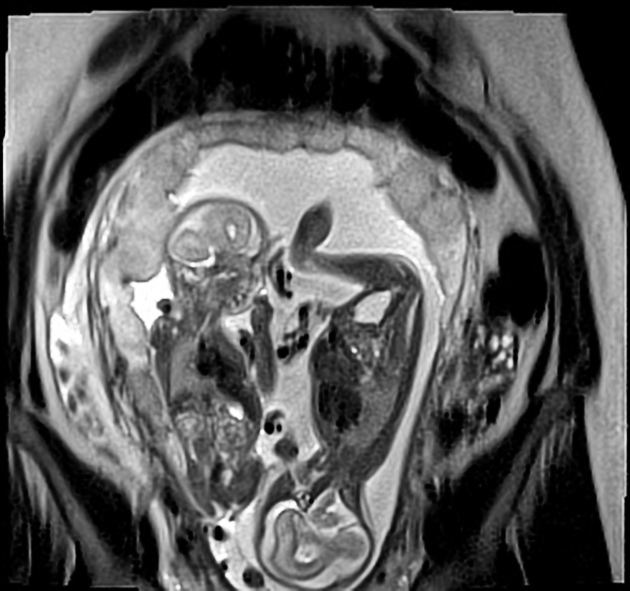
TTTS results from unbalanced vascular (arteriovenous and arterioarterial) anastomoses in the placenta - that is, placental circulation is directed predominantly towards one twin and away from the other.
The resultant hypovolemia and hypoperfusion in one twin and hypervolemia and hypertension in the other create a cascade of hormonal changes including the renin-angiotensin system. This in turn leads to chronic tubulopathy and oliguria in the hypovolemic (donor) twin with consequent oligohydramnios, and polyuria and consequent polyhydramnios in the hypervolemic (recipient) twin.
Staging
The extent of the syndrome can be staged according to severity. One method proposed by Quintero et al. is as 3:
stage I: oligohydramnios/polyhydramnios
stage II: bladder not visible in donor twin
stage III: abnormal Dopplers in either twin
stage IV: hydrops fetalis in either twin *
stage V: in utero demise of either twin
* Almost always in the recipient; rarely in the donor if there is coexistent TAPS (see below).
Variants
Twin anemia-polycythemia sequence (TAPS) is a described subset of TTTS, which is discussed separately.
Radiographic features
Ultrasound
Monochorionicity is a prerequisite at any stage of gestation.
Growth discordance is often but not invariably present, and does not contribute to diagnostic criteria.
First trimester
The following findings on a first-trimester ultrasound of a monochorionic pregnancy have been associated with an increased risk of developing TTTS, although predictive value remains poor 8:
NT discordance: 20% or more
CRL discordance: 10% or more
folding of the inter-twin membrane as an early sign due to a disparity in amniotic fluid volumes (amniotic fluid discordance)
Second and third trimesters
Features that may be noted individually in each twin include:
-
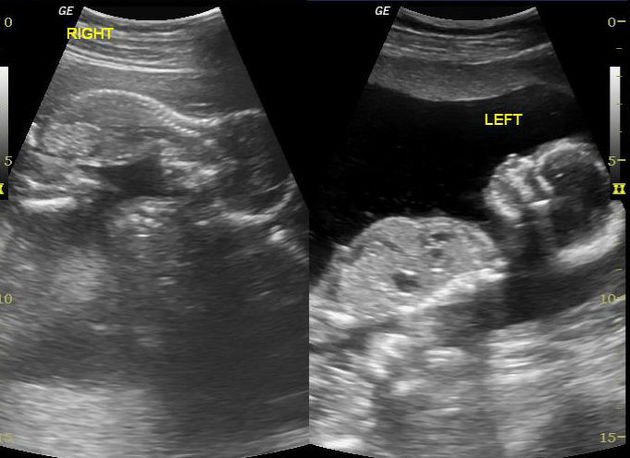
recipient twin
large or constantly cycling urinary bladder
-
features of cardiac overload
-
in certain cases, fetal echocardiography may also show AV valve incompetence
Doppler abnormalities: predominantly venous
-
donor twin
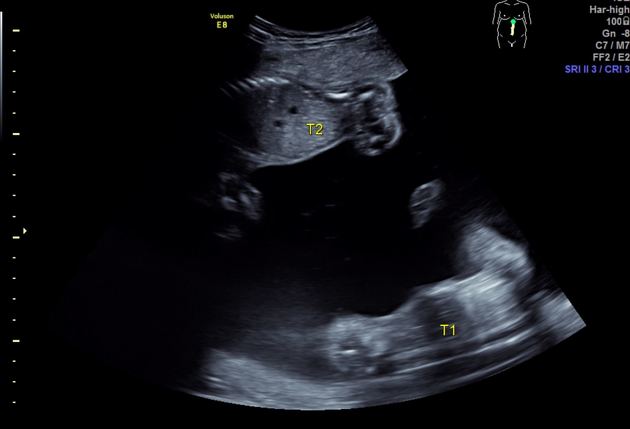
oligohydramnios (deepest vertical pocket <2 cm), causing the twin to appear pinned to the edge of the chorion, the so called "stuck twin"
small or non-visualized urinary bladder
Doppler abnormalities: predominantly umbilical artery +/- venous
evidence of fetal anemia
Color Doppler
absent or reversed diastolic flow in the umbilical artery is an indication of worsening twin-to-twin transfusion syndrome
abnormal ductus venosus waveform pattern suggests the possibility of cardiac diastolic dysfunction
Treatment and prognosis
Serial sonographic monitoring is common practice. In an uncomplicated monochorionic twin pregnancy, TTTS screening should start from 16 weeks gestation with assessment of fetal growth, deepest vertical pockets, and umbilical arterial pulsatility index (UA-PI) performed every two weeks. Detailed morphology ultrasound is routine at 20 weeks. Additional fetal middle cerebral arterial-peak systolic velocity (MCA-PSV) is recommended from 22 weeks.
Untreated, TTTS generally carries a poor prognosis, with up to 90% perinatal mortality 8. Laser coagulation of the chorionic plate is the treatment of choice and significantly improves the prognosis for both twins - although both morbidity and mortality remain considerably higher than in non-TTTS monochorionic pregnancies.
Other management options include:
conservative management with surveillance for Quintero stage I TTTS
serial amnioreduction, where laser treatment is not available 8
Differential diagnosis
General imaging differential considerations include:
other causes of oligohydramnios and/or polyhydramnios, e.g. related to fetal structural anomalies
isolated placental insufficiency in one of the twins (will not produce polyhydramnios in the other twin)






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.