Uterine arteriovenous malformations (AVMs) result from the formation of multiple arteriovenous fistulous communications within the uterus without an intervening capillary network.
On this page:
Terminology
Somewhat confusingly, the term “uterine arteriovenous malformation” has been used interchangeably with “enhanced myometrial vascularity” in the literature. The terms have been used to describe the sonographic appearance of a hypervascular lesion within the uterine myometrium that demonstrates turbulent flow. However, there is a growing understanding that they represent separate pathological entities 16,17. Thus at the 2015 annual World Congress of the International Society of Ultrasound in Obstetrics and Gynecology (ISUOG), it was recommended that “enhanced myometrial vascularity” is the preferred term for what was previously known as an “acquired uterine arteriovenous malformation” 18. The recommendation was made as most of these cases do not represent true arteriovenous malformations 18.
For more details, see the article on enhanced myometrial vascularity. The remainder of the article pertains to true uterine arteriovenous malformations.
Epidemiology
Associations
Uterine arteriovenous malformations are rare and can either be congenital or acquired 15. Acquired arteriovenous malformations are more common and are associated with conditions such as 4,7:
- multiple pregnancies
- miscarriage
- previous surgery
- dilation and curettage
- termination of pregnancy
- cesarean section
Clinical presentation
The presentation of uterine arteriovenous malformations varies. Uterine bleeding is the major presenting symptom, and it may be massive and life-threatening in young women. As these malformations are less common after menopause, post-menopausal bleeding is rarely seen. Congestive heart failure secondary to a vascular steal syndrome can be a less common clinical manifestation with a large uterine arteriovenous malformation.
Pathology
A uterine arteriovenous malformation consists of a proliferation of vascular channels with fistula formation and an admixture of small, capillary-like channels. The size of these vessels can vary considerably. They are classified as congenital or acquired.
Congenital uterine arteriovenous malformations tend to have multiple feeding arteries, a central nidus (a tangle of vessels with histologic characteristics of both arteries and veins), and numerous large draining veins 6.
Acquired or traumatic uterine arteriovenous malformations (also called arteriovenous fistulas) represent multiple small arteriovenous fistulas between intramural arterial branches and the myometrial venous plexus 7. They typically represent a single artery joining a simple vein.
Radiographic features
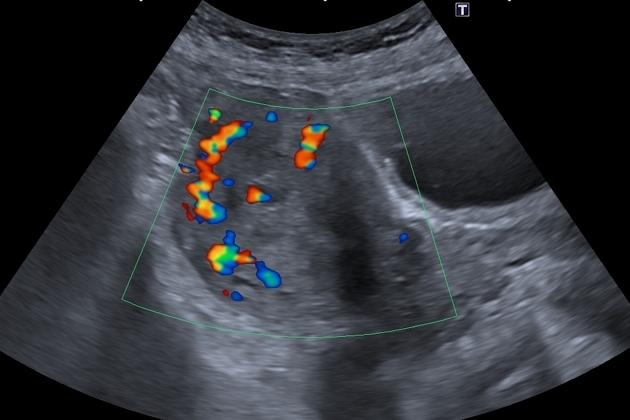
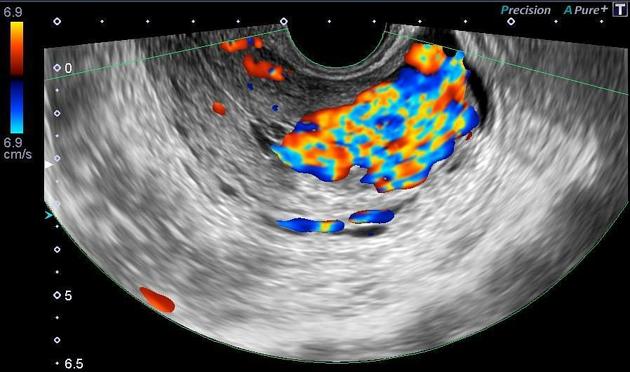
Ultrasound
Greyscale sonographic appearances can be non-specific with a range of manifestations including areas of subtle myometrial inhomogeneity, tubular spaces within the myometrium, an intramural uterine, endometrial or cervical mass like region or sometimes as prominent parametrial vessels 2. The extent of the mass effect, however, is minimal.
Color Doppler ultrasound typically shows a low resistance (RI ~0.2-0.5), high-velocity flow pattern.
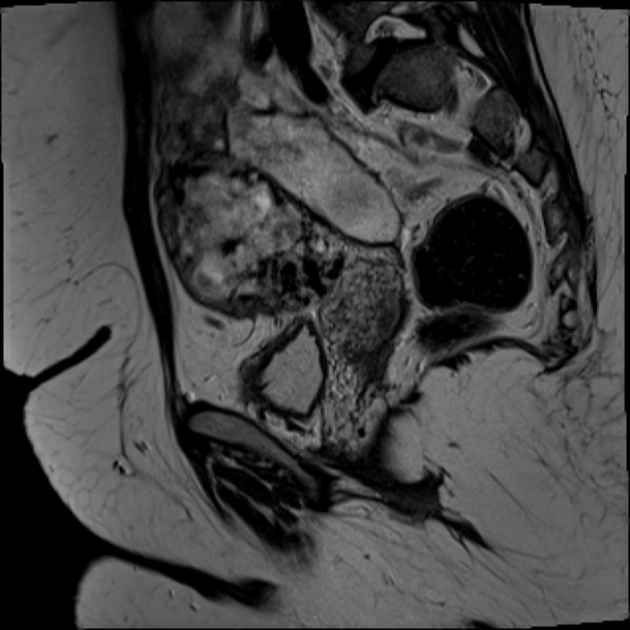
MRI
MRI shows multiple serpentine flow-related signal voids typically seen in the uterine wall, endometrial cavity, and parametrium on T1 and T2 weighted images. Contrast-enhanced dynamic MR angiography can depict complex serpentine abnormal vessels that enhance as intensely as normal vessels and show early venous return 4.
Angiography (DSA)
Digital subtraction angiography (DSA) shows a hypervascular lesion with early venous filling. Conversely, enhanced myometrial vascularity will show a hypervascular lesion without early venous filling 15.
Treatment and prognosis
Transcatheter arterial embolization is an excellent treatment option in selected cases ref.
History and etymology
They were first described by G Dubreil and E Loubat in 1926 3.
Differential diagnosis
The primary differential diagnosis on ultrasound imaging appearances is enhanced myometrial vascularity. This can be distinguished on DSA.
If serum beta-HCG is elevated, consider:
- gestational trophoblastic disease (GTD)
- retained products of conception (RPOC): abnormality centered on endometrium rather than myometrium 14






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.