Uterine artery embolization (UAE) is an interventional radiological technique to decrease the arterial supply to the uterus and is performed for various reasons.
On this page:
History
Uterine artery embolization has been practised for more than 20 years for controlling post-partum hemorrhage.
The technique was first reported as an effective intervention for fibroids in 1995 when Ravina et al noted that several women with symptomatic leiomyomata who underwent uterine artery embolization as a pre-hysterectomy treatment had significant clinical improvement to an extent that hysterectomy was no longer required.
It is now estimated that more than 100,000 UAE procedures have been performed for the treatment of fibroids.
Indications
-
uterine fibroids (intramural, submucosal, and subserosal)
pelvic pain and pressure/fullness
mass effect symptoms such as urinary frequency, bladder outlet obstruction and hydronephrosis due to ureteric compression
fibroids with otherwise undiagnosed infertility
as a preoperative technique to decrease the size of large fibroids
post-partum hemorrhage
-
other less common indications include
uterine AVM: trauma, post curettage
if active extravasation of contrast is detected during angiography for another reason (post-trauma)
Patients with fibroids, and their related problems, probably present the largest group who is most able to benefit from uterine artery embolization. Presently people with multiple and/or large symptomatic uterine fibroids traditionally undergo total abdominal, vaginal or laparoscopic-assisted hysterectomies around the world. The figure in the United States is about 60,000 hysterectomies per year. In less developed and more populous countries like India, the numbers may be even higher. There is an increasing need for minimally alternatives for uterine fibroids and dysfunctional bleeding.
Contraindications
-
contraindications to angiography
uncorrectable coagulopathy
severe renal insufficiency
current pregnancy
active pelvic infection
connective tissue disease (relative)
prior surgery with adhesions (relative)
In addition, many gynecology societal guidelines do not recommend performing UAE on women who maintain a future desire for pregnancy. Exceptions to this may include women who have severe anemia or symptoms associated with fibroids, have failed conservative measures and have contraindications to surgery or those who consent to UAE within an approved research protocol. However, recent studies have shown that fertility and miscarriage rates after uterine artery embolization for fibroids are likely similar to the age-matched general population11.
Procedure
Preprocedural evaluation
a thorough gynecological history and examination covering the patient's symptoms and goals of treatment
pelvic ultrasound and MRI
up-to-date cervical screening
consider endometrial biopsy if there are concerning clinical or imaging features
relevant history of other medical problems
allergies
Equipment
Catheter selection
Any catheter suitable for contralateral and ipsilateral uterine artery cannulation
Roberts uterine catheter (RUC): commonly used selective catheter for pelvic angiography
Cobra glidecath: can also be used
right internal mammary catheter: may be used, but less common
microcatheters may be used to cannulate smaller caliber arteries
Embolic agents
The type of embolic agent selected will depend on the indication.
-
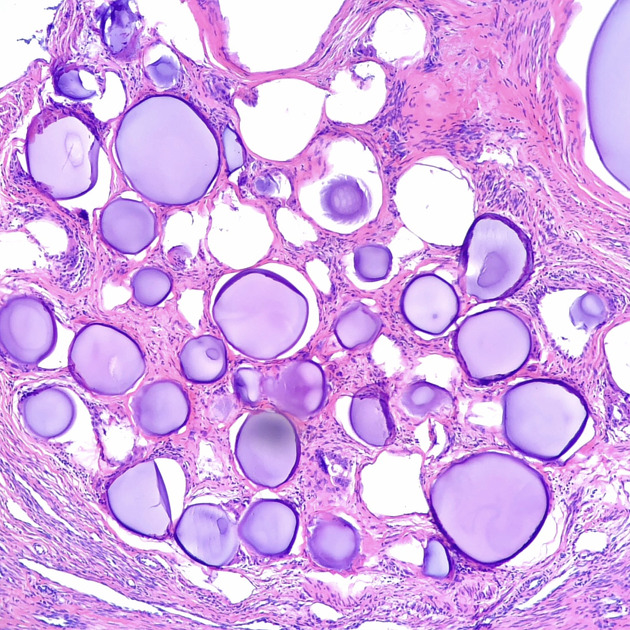
fibroids and adenomyosis
PVA (typically 300 - 500 or 500 to 700 µm)
Embosphere® microspheres
-
gel foam slurry
n-butyl-cyanoacrylate (glue)
Technique
The approach is dependent on operator preference.
Femoral access
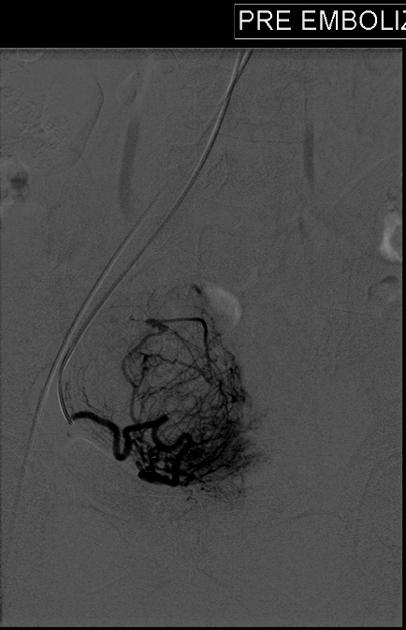
The contralateral internal iliac artery is selected. The uterine artery is a branch of its anterior division and has a distinctive radiographic appearance. Care is taken to avoid cervical and vaginal branches, this is usually avoided by selective catheterization of the uterine artery distal to the origin of these branches.
The ipsilateral uterine artery is selected, commonly by formation of a Waltman loop, and subsequent embolization performed.
Embolization endpoint is diminished forward flow or near-stasis of the main uterine artery trunk.
The ovarian arteries and inferior mesenteric artery may also be interrogated and if fibroid vascularity is detected these may also be embolized.
Brachial or radial access
This is typically performed via the left upper limb. In general, this technique allows for easier uterine artery selection, however, it presents challenges regarding catheter length and there is a small risk of stroke as the catheter crosses the origin of the left vertebral artery.
Peri-procedural care
IV sedation is commonly given by the treating interventional radiologist or anesthetic team
patients may be required to stay in hospital overnight to ensure adequate pain relief
-
analgesia
-
local anesthesia
intra-arterial local anesthetic injection has been described 12
-
IV fluids
antiemetics
antibiotics
Intravenous fluids, analgesia, antiemetics and antibiotics need to be continued during the postprocedural period.
Complications
-
angiography complications
sepsis is a rare but serious complication and can be difficult to differentiate from post embolization syndrome.
vaginal expulsion of fibroid tissue
fibroid fragment retention
pregnancy outcomes are uncertain after uterine artery embolization
Outcomes
For post-partum bleeding
prevents the need for emergency hysterectomy
retain fertility after UAE for postpartum hemorrhage (PPH) compared to hysterectomy
For fibroids
menorrhagia/dysmenorrhea and metrorrhagia improve in 70-95% of cases
shorter hospital stay and recovery period that hysterectomy and myomectomy
hospital stay is rarely >48 hours
patients are often back to work within 10 days
no post laparotomy complications
mean uterine volume reduction by 26-59%
fibroid volume reduction by 40-75% (after 6-12 months)
the overall complication rate is approximately 10% for minor complications, with major complications at 1.5%
low rate of uterine infection as a complication (<2.5%) and very low rate of infection requiring hysterectomy (<0.7%) 13
In a study of follow up two and four years after uterine artery embolization or myomectomy, women with symptomatic uterine fibroids were likely to have mildly better health quality of life results with myomectomy than uterine artery embolization at two years, but equivalent outcome at four years 10,14.
For adenomyosis
In studies of follow up after uterine artery embolization for adenomyosis, 74-82% of women with symptomatic adenomyosis had sustained improvement in quality of life scores and avoided hysterectomy 16.
Recommendations
American College of Obstetrics and Gynecology (ACOG) 2021 Practice Bulletin: UAE is recommended as an interventional procedure for the treatment of uterine leiomyomas in patients who desire uterine preservation and are counseled about the limited available data on reproductive outcomes 9
NICE (UK) uterine artery embolization for fibroids 2010: UAE is efficacious for symptom relief in the short and medium term for a substantial proportion of patients 15










 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.