Dual-energy CT has a variety of clinical applications in vascular imaging, due to the utilization of material decomposition and the ability to reconstruct images at a variety of energy levels.
Clinical applications
High kVp CT scans have lower contrast than that of lower kVp due to the K-edge of iodine, giving the lower energy of the dual energy scan an advantage over conventional CT. The attenuation values of large vessels enhanced with iodine are 70% higher at 80 kVp than at 140 kVp 1. In the event of suboptimal contrast injection and or timing, the lower energy set (closer to the K-edge of iodine) can be favored to improve the contrast resolution in various studies from pulmonary angiograms to aortograms 2.
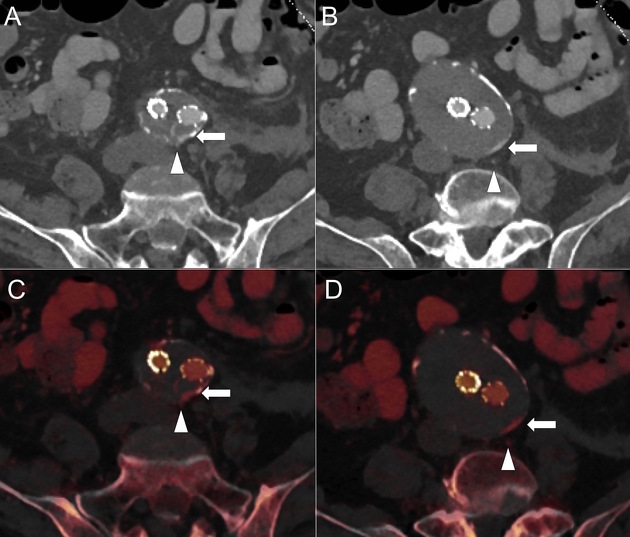
EVAR surveillance
Dual-energy aortogram in surveillance of endovascular aneurysm repair improves detection of endoleaks in fewer acquisitions 1; low kVp scanning can detect subtle leaks, while the virtual non-contrast images replace the unenhanced scan allowing a substantial reduction in radiation burden in patients that require life-long checkups 3,4.
Contrast sparing
Using lower energy data sets are proven to increase the arterial enhancement of pulmonary angiograms and other contrast studies due to the K-edge of iodine being closer to the lower energy used in a dual energy scanner 5-7.
Pulmonary angiography
The 80 kVp image has the potential to improve subsegmental pulmonary artery perfusion and distal pulmonary embolus detection 2. In the setting of suboptimal enhancement of the pulmonary artery, virtual monochromatic reconstructions at lower energy levels can increase vessel enhancement, at the cost of increased noise.
Perfusion blood volume maps can be used to identify the segmental or subsegmental areas of the lung affected by a pulmonary embolus. It is important to note that atelectasis, cardiac motion and streak artifact can all cause perfusion defects 10.






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.