Presentation
Abdominal pain.
Patient Data
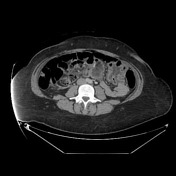






Antecolic bypass with gastric sleeve and duodenal switch. The proximal roux limb makes a rapid leftward turn into a cluster of mildly thickened jejunum in the left mid-abdomen, which on coronal images has a C-shaped configuration with mesenteric edema converging toward the midline. The mucosa is mildly hyperenhancing. The jejunum exits this cluster just before the jejunojenostomy. Small amount of ascites.

Annotated coronal image highlights a few key findings.
Case Discussion
This patient has a history of failed vertical banded gastroplasty converted to a duodenal switch. Teaching points:
- when reviewing the axial images, there is a clustered appearance of the small bowel in the left mid-abdomen with mesenteric edema and minor swirling of the vasculature
- coronal reformats allow you to see the internal hernia en face, allowing you to more confidently visualize the involved proximal jejunum with wall thickening + mesenteric edema, as well as see the vasculature converging toward the hernia defect
- thus this case is a good reminder to use all reformats to try to understand complex bowel cases, and appropriately be concerned about a risk of internal hernia in a patient with a history of bypass when you see clustered bowel, mesenteric edema, and swirling/narrowing of the vasculature
Operative note excerpt: "Anatomy consistent with a duodenal switch. There was a patulous jejunojejunostomy with a large mesenteric defect at the site of the anastomosis, and a portion of the small bowel had herniated through this defect. During the running of the alimentary limb, we reduced the small bowel through the defect. All bowel appeared healthy and noncongested with appropriate blood flow...we then inspected the mesenteric defect at the site of the enteroenterostomy and this appeared quite large. The defect was closed..."




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.