Presentation
Presenting through ER with jaundice and elevated blood sugar 160 mg/dL. Known to have Alzheirmer's disease.
Patient Data
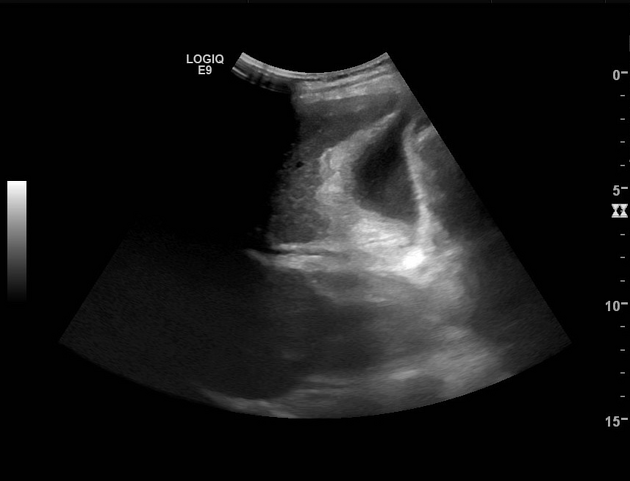
The liver shows normal echogenicity and echotexture, no visible focal lesions or megaly. It measures 13.5 cm.
The gallbladder shows pericholecystic edema and wall thickening measures 1 cm with no evidence of stones, findings are indicating reactionary cholecystitis. Thickening and increased echogenicity of the intrahepatic biliary tree is also seen suggesting acute cholangitis.
No intra or extra hepatic biliary dilatation.
Multiple renal cysts seen bilaterally, the largest at the right inter-polar region measuring 5.3 cm.
Rest of the examination was normal. (images not included)

Heterogeneous hypoechoic geographic areas are seen suggesting infection.
Rest of the examination was normal. (images not included)

The previously noted heterogeneous hypoechoic geographic areas are still noted suggesting infection but no liquefication or abscess formation now.
Rest of the examination was normal. (images not included)
Case Discussion
Acute cholangitis is a clinical diagnosis. On ultrasound examination, the hallmark finding is thickened walls of the biliary ducts although this is non-specific. However, it is essential to identify biliary obstruction by stones (choledocholithiasis) and pus may also be identified as debris material within the common bile duct if present. In our case, clinical and laboratory evaluation confirmed ascending cholangitis, and repeated abdominal ultrasound examinations were requested after admission due to slowly responding high-grade fever.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.