Presentation
Abdominal pain and vomiting.
Patient Data






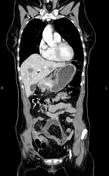



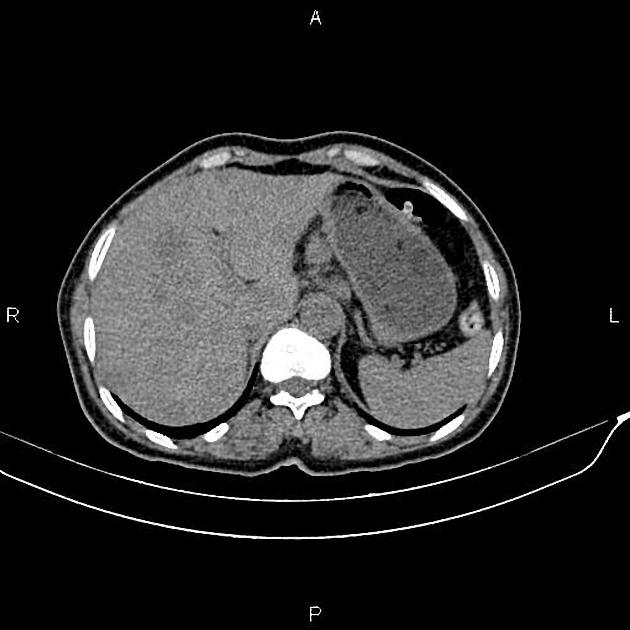
Increased wall thickness due to tumoral infiltration is present at gastric antrum and pylorus accompanied by multiple peri gastric lymphadenopathies with maximum SAD of 20mm. In addition, numerous ill-defined low enhancing masses are seen throughout the liver less than 35mm.
A 33mm cystic lesion is noted at right adnexa.
There is also a little free fluid at posterior cul-de-sac.
Case Discussion
Gastric mass (path proven adenocarcinoma) with regional lymphadenopathies and diffuse hepatic metastasis.
CT is currently the staging modality of choice because it can help identify the primary tumor, assess for the local spread, and detect nodal involvement and distant metastases.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.