Presentation
2-3 month hx recurrent sudden onset, severe, sharp headaches. Onset while weightlifting, Uncertain severity or time to max severity. Recurrent on Valsalva - laughing, sneezing, bending forward, also on lying flat. Recently nausea and vertigo lying flat. Nil focal on examination.
Patient Data


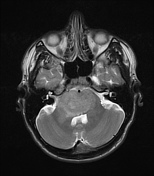

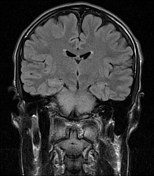

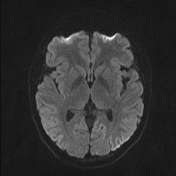



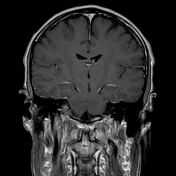

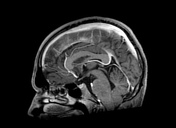

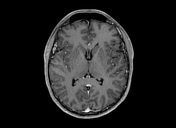


Right paramedian pontine tumor. It extends across the midline occupying the ventral portion of the pons. RIght cerebral and middle cerebellar peduncle extension.
No brain or spinal (not uploaded) metastases.
Macroscopy
The specimen consists of six cores of pale tissue.
Microscopy
Sections show cores of neural tissue comprising white matter and brainstem nuclei, including scattered pigmented neurons. The neuropil appears somewhat vacuolated in areas (likely biopsy artefact). There is no significant hypercellularity. Background astroglia show mild pleomorphism but no significant nuclear atypia. Mitotic figures are not identified. There is no apoptosis, vascular proliferation or necrosis. No Rosenthal fibers or eosinophilic granular bodies are identified.
GFAP highlights the astroglial cell population. Staining for the common mutated form (R132H) of IDH-1 is positive in a notable number of cells. ATRX is suboptimal, making meaningful interpretation difficult; however, loss of staining is observed in a proportion of cells. H3K27M is negative. Strong nuclear expression of p53 is noted, focally. The tumor cells are negative for NeuN. The MIB1 proliferative activity is low, staining sparse, scattered cells.
Comment
Although no solid tumor is identified in the material examined, staining for IDH-1 does reveal a diffusely infiltrative population of tumor cells. As such, the features in these small biopsies are consistent with a diffuse astrocytoma, IDH-1 mutant, WHO grade 2.
Brain stem biopsy - Diffuse astrocytoma, IDH-1 mutant, WHO grade 2
Case Discussion
This case highlights the importance of determining where a brainstem tumor is centered in pediatric patients.
What used to be called a diffuse brainstem glioma, now referred to by the mutation H3K27M, is a tumor that is almost always midline and ventral. An alternate diagnosis should be considered when the tumor is centered off-midline or does not involve the ventral brainstem.
In this case, the tumor is right para-median and dorsal. While it does spread into the brainstem and involve the ventral brainstem, that is not its epicenter. Biopsy confirmed adult-type astrocytoma IDH mutant.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.