Presentation
The patient presents with acute onset of hypoxia and tachypnea during and post general anesthesia.
Patient Data

The portable chest X-ray demonstrates extensive, ill-defined, bilateral ground glass opacity and infiltrates. There is a wide differential diagnosis including ARDS, cardiogenic and non-cardiogenic pulmonary edema, and atypical infection including COVID-19 pneumonia and PJP.



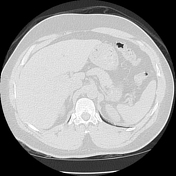
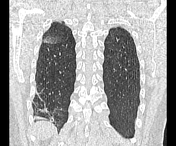
CT scanogram demonstrates persistent infiltrates. There is however significant radiological improvement with supportive fluid, antibiotic and oxygenation therapy within 22 hours of the initial anesthetic.
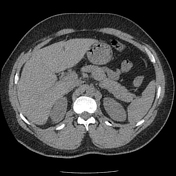

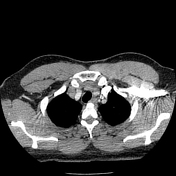




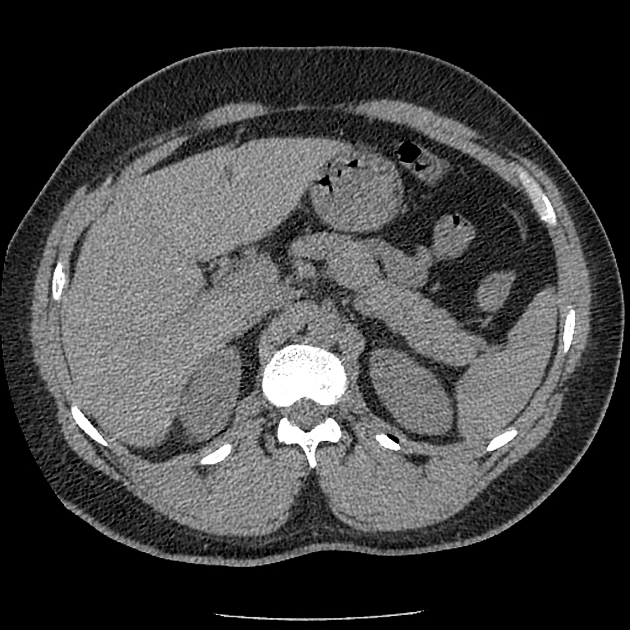
There is a type I sliding hiatal hernia with fluid and gastric contents within the esophagus suggesting gastro-esophageal reflux and alluding to the cause of the acute aspiration pneumonitis experienced during general anesthesia. There is intermittent reflux even between the non-contrast and post-contrast phases in a recumbent position during CT performance as demonstrated within the esophagus between the 2 phases.
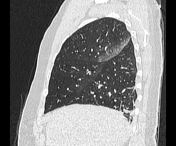
There are typical changes with the posterior and dependent segments of the right upper lobe, right middle lobe, and left upper lobe including the singular segment. These include a combination of tree-in-bud within the left upper lobe, and ground glass opacity within the rest of the affected segments.
There is subsegmental atelectasis within the right lower lobe often a normal post recent anesthetic finding.
There are no aspirated contents within the airways.


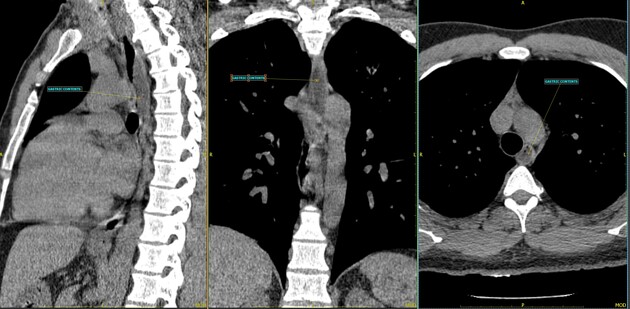
Reformated and annotated images show the type I sliding hiatal hernia and gasto-oespohageal reflux with a variable volume of gastric contents within the upper thoracic esophagus.
Case Discussion
A case of acute aspiration pneumonitis and more specifically aspirated gastric contents (Mendelson syndrome ) during a general anesthetic. The patient underwent a short-duration general anesthetic for the surgical excision of a dermatological mass. The presence of a sliding hiatal hernia and gastro-esophageal reflux during a recumbent position during general anesthesia contributed to gastric content aspiration.
The CT study confirms significant resolution of the pulmonary infiltrates within a relatively short duration of time and obviated the need for aggressive management and intubation.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.