Presentation
History of hemoptysis and coma 2 months ago. Liver cirrhosis by US. She had an old history of cholecystectomy.
Patient Data










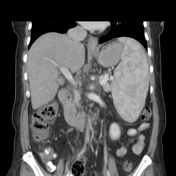



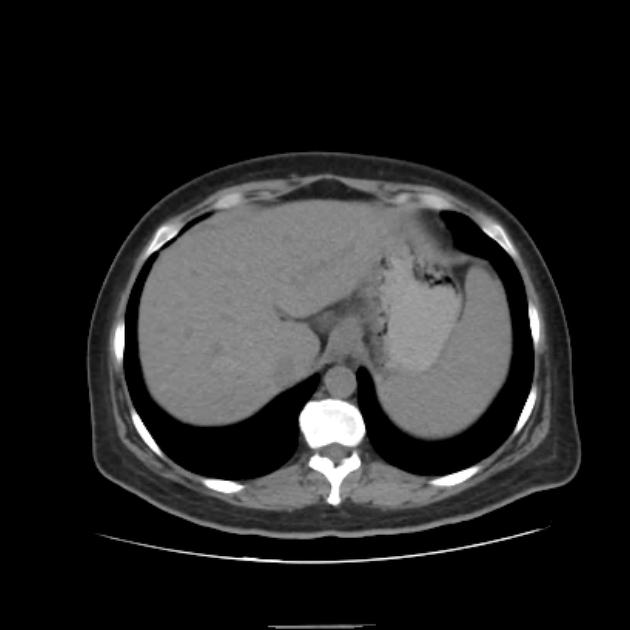
Liver cirrhosis evident by hypertrophied caudate lobe and prominent interlobar fissures. The liver shows coarse trabecular parenchymal pattern. Mild periportal edema is noted. No hepatic focal lesions. Patent portal vein and its branches. Splenomegaly. Bulky pancreas. Multiple enlarged celiac, porta-hepatis and portocaval lymph nodes. Soft tissue sheets are encasing the superior and inferior mesenteric arteries.
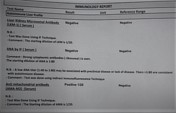
Autoimmune markers revealed elevated antimitochondial antibody (AMA-M2)
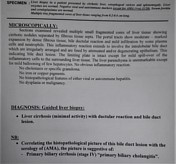
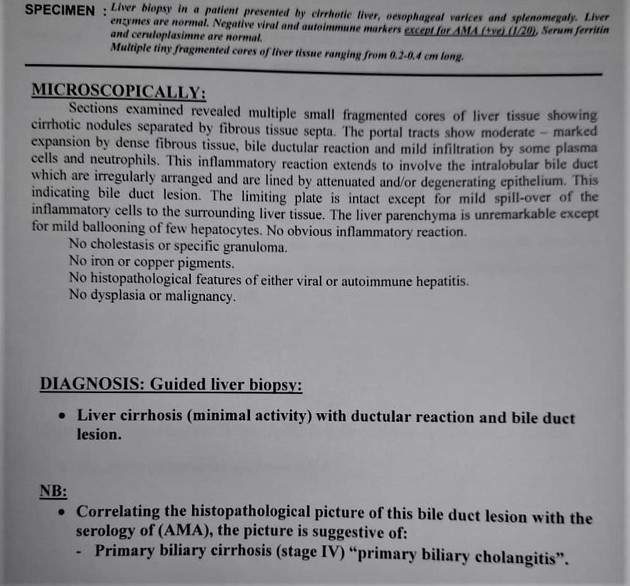
Liver biopsy revealed primary biliary cholangitis.
Case Discussion
The patient had negative markers for hepatitis B and C viruses, yet she had liver cirrhosis with coarse trabecular parenchyma and enlarged porta-hepatis and poro-caval lymph nodes, which raised the possibility of autoimmune hepatitis. Soft tissue sheets encasing the superior and inferior mesenteric arteries raised the possibility of vasculitis commonly seen in autoimmune disease or IgG4. The patient tested positive for serum antimitochondrial antibody (AMA-M2) which is highly sensitive and specific for primary biliary cholangitis. Liver biopsy revealed primary biliary cholangitis.
Autoimmune liver diseases are classified into:
- autoimmune hepatitis (AIH)
- primary sclerosing cholangitis (PSC)
- primary biliary cirrhosis (PBC)
Primary biliary cholangitis (PBC) is common in middle-aged women presenting with symptoms of fatigue and pruritus and laboratory test evidence of cholestasis.
It could be associated with other autoimmune diseases such as Sjögren syndrome (~75%), autoimmune thyroiditis (~25%), systemic sclerosis.
Laboratory work up: serum anti-mitochondrial antibody (AMA) is highly sensitive and specific for primary biliary cholangitis
Radiographic features of PBC include:
- T2: if parenchymal lace-like fibrosis and periportal halo sign are both highly sensitive for PBC
- periportal hyperintensity (cuffing)
- segmental hypertrophy, notably of the caudate lobe
- hepatic surface irregularity due to regenerative nodules
- regional lymphadenopathy: tends to dominate in the gastrohepatic ligament and porta hepatis
- splenomegaly




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.