Pulmonary artery aneurysms following surgery for Tetralogy of Fallot
Presentation
Chest pain and shortness of breath.
Patient Data

Right-sided aortic arch. Left hilar 'mass'. No normal main pulmonary artery identified on either side. Small sternotomy wires. No focal airspace opacity. No pleural effusion.
Following the receipt of the chest x-ray report, the clinical team provided further information:
He had repair for Tetralogy of Fallot as a child and has not been under regular cardiology follow-up. He had a right ventricle to pulmonary trunk conduit, with recent the most recent echocardiogram finding pulmonary stenosis and regurgitation.


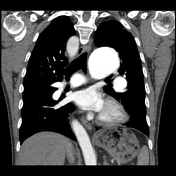

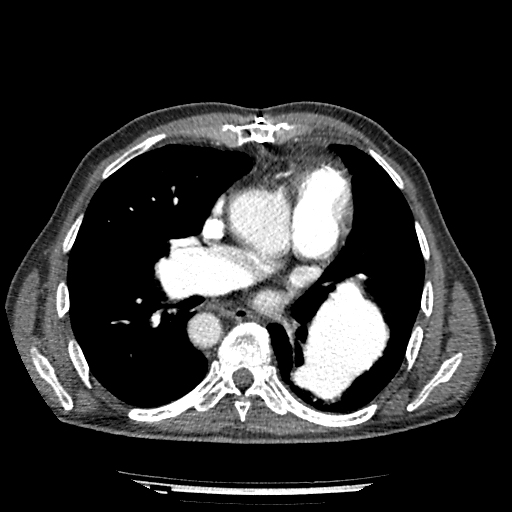
No pulmonary embolism. Gross dilatation of the left and right main pulmonary arteries. Abrupt change of caliber to relatively normal lobar and segmental level vessels. Right ventricular dilatation and hypertrophy. Right-sided aortic arch. No airspace opacities. No pleural or pericardial effusion.
Following cardiology work-up which identified worsening pulmonary stenosis and regurgitation, but no ventricular septal defect, the patient had pulmonary outflow tract stent placement.
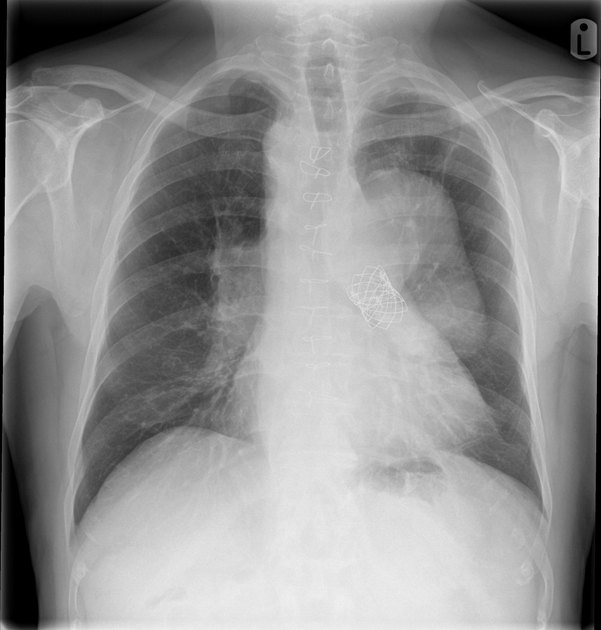
Right-sided aortic arch. Left hilar 'mass'. Metallic stent projected to left of midline, known to be a pulmonary valve stent. Small sternotomy wires. No focal airspace opacity. No pleural effusion.
Case Discussion
The patient had surgery many decades earlier for Tetralogy of Fallot, and was not under regular follow-up. This history was not elicited at the time of presentation. The initial CXR picked up hilar 'masses', and when combined with the finding of an aortic arch and small sternotomy wires, an astute reporter may make the diagnosis of a treated congenital cardiac disease. This was indeed the case, with the patient having had an RV to PA conduit, and then subsequently developed pulmonary stenosis and regurgitation. This led to the pulmonary artery dilatation and RV hypertrophy and dilatation. No VSD was identified. He was treated with pulmonary valve stenting.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.