Presentation
Patient with a history of metastatic papillary thyroid carcinoma undergoing immunotherapy, who underwent a renal biopsy to evaluate rapidly progressive renal failure. Following the procedure, the patient developed hematuria and anemia.
Patient Data




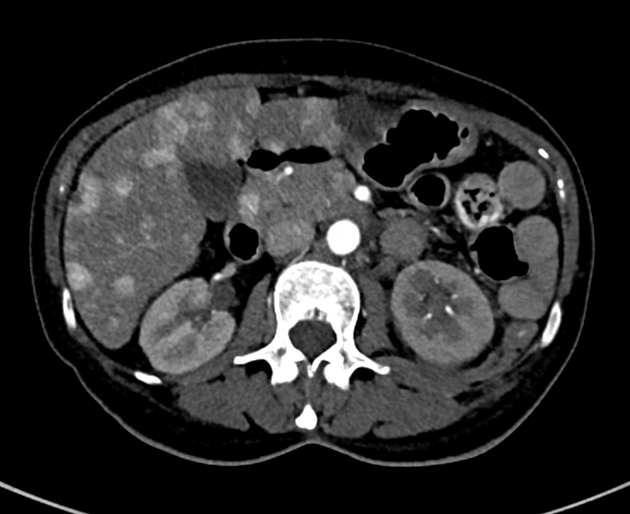
Computed tomography (CT) was performed due to suspected active bleeding, which was ruled out.
The early enhancement of the left renal vein is observed up to its confluence with the inferior vena cava, along with enhancement of its distal branches towards the lower pole. A direct communication with a distal branch of the renal artery is identified, consistent with an arteriovenous shunt.
In the liver, spleen, and pancreas, multiple heterogeneous lesions are noted, some of which exhibit arterial-phase hyperenhancement, suggestive of metastatic disease (M1).


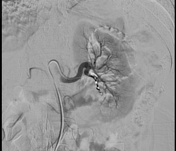

A fluoroscopic study reveals catheterization of a distal branch of the left renal artery, with contrast passage and early enhancement of the renal vein and inferior vena cava.
A fluoroscopic study after the application of a selective coil in the distal branch of the left renal artery showed no further communication with the venous system.
Case Discussion
Renal arteriovenous fistulas (RAVFs) are rare vascular complications with an incidence ranging from 1% to 18%, with particular relevance to their occurrence following renal biopsy, as it accounts for up to 70% of cases.
These fistulas result from abnormal communication between an artery and a vein within the renal parenchyma, typically due to trauma to both vessels during the procedure.
They can present as asymptomatic or lead to severe complications, as in our case, where the fistula was associated with frank hematuria, hypotension, and hemodynamic instability, necessitating urgent endovascular treatment. Selective coil embolization was successfully performed, cutting off the shunt flow and stabilizing the patient.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.