Anterior shoulder dislocation is by far the commonest type of dislocation and usually results from forced abduction, external rotation and extension 1.
On this page:
Epidemiology
Broadly speaking, anterior shoulder dislocations occur in a bimodal age distribution. The first, and by far the more prevalent age group are young adult men who have sustained high-energy injuries to the shoulder. The second group is older patients who have been injured with a much lower level of violence. In older patients, the dislocation usually proves to be an isolated event 2.
Predisposing factors
flattened, shallow anterior/anteroinferior glenoid bony contour: may predispose to recurrent dislocations 3
Radiographic features
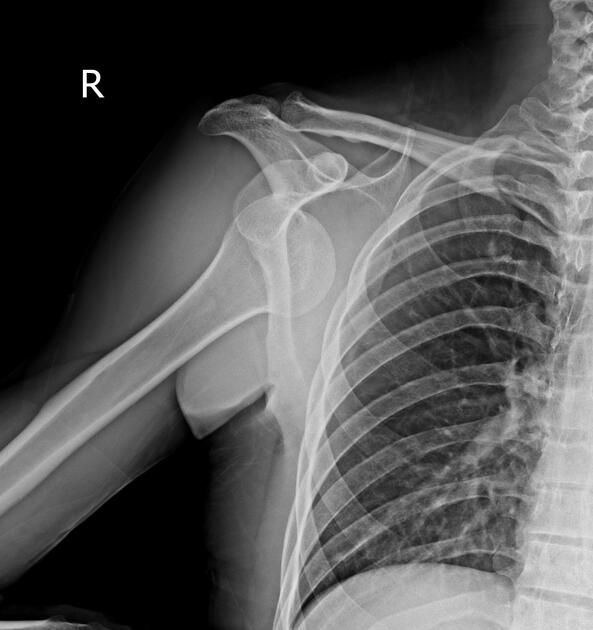
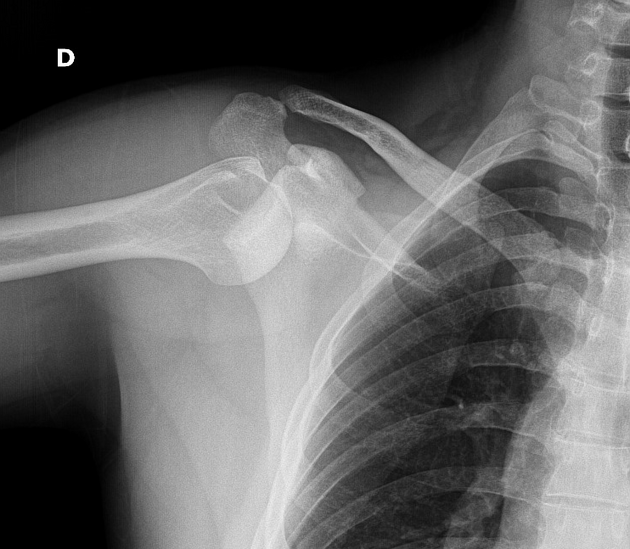
Anterior dislocations can be further divided according to where the humeral head comes to lie:
subcoracoid: most common
subglenoid
subclavicular
intrathoracic: very rare
In anterior dislocations, the humeral head comes to lie anterior, medial and somewhat inferior to its normal location and glenoid fossa.
Treatment and prognosis
Anterior shoulder dislocations are usually managed with closed manual reduction and a period of immobilisation (e.g. 6 weeks) to allow adequate capsular healing, although whether this significantly changes the likelihood of recurrent dislocation is not certain 4. The key to successful healing and normal eventual function is a structured course of physiotherapy aimed at reducing muscle wasting and maintaining mobility. The emphasis, especially early on, is on isometric exercises, in which the glenohumeral joint remains immobilised 4.
Surgical repair is not required for dislocation per se, but rather to treat complications and associated injuries which include:
shoulder instability due to damage to the inferior glenohumeral ligament (IGHL)
damage to the axillary artery, or brachial plexus




















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.