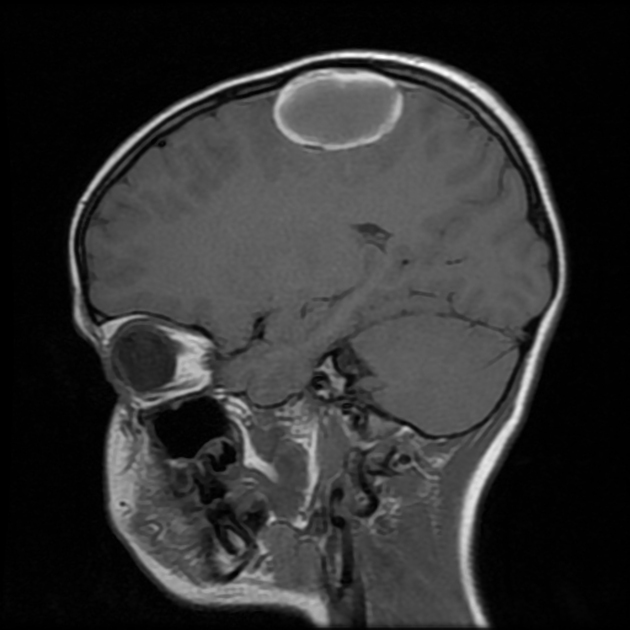
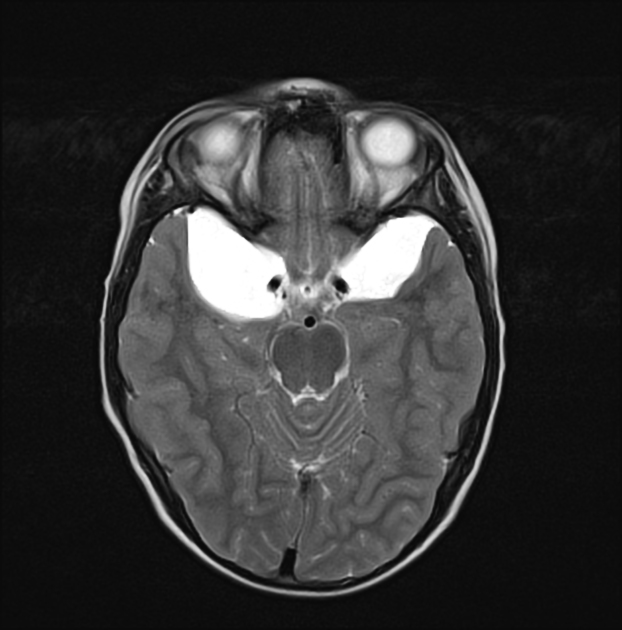
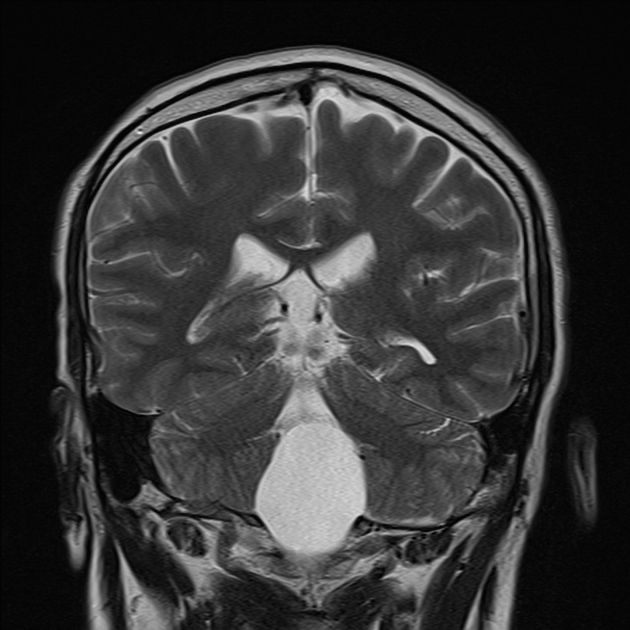
Arachnoid cysts are relatively common benign and asymptomatic lesions occurring in association with the central nervous system, both within the intracranial compartment (most common) as well as within the spinal canal. They are usually located within the subarachnoid space and contain CSF.
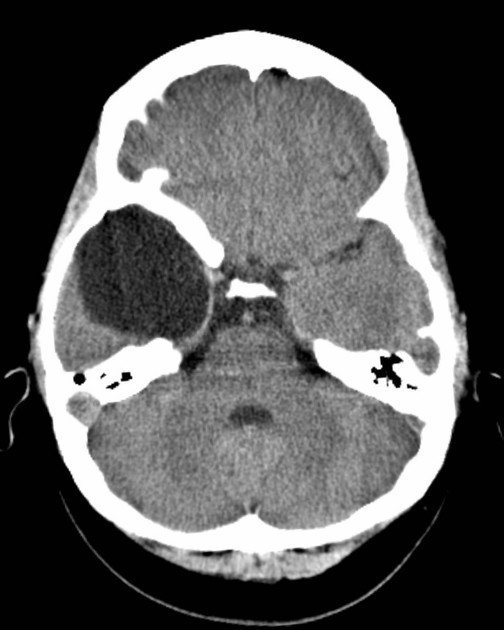
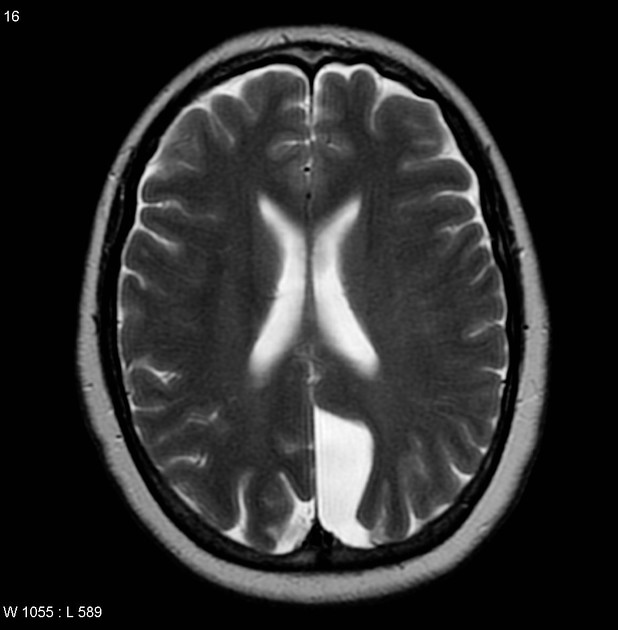
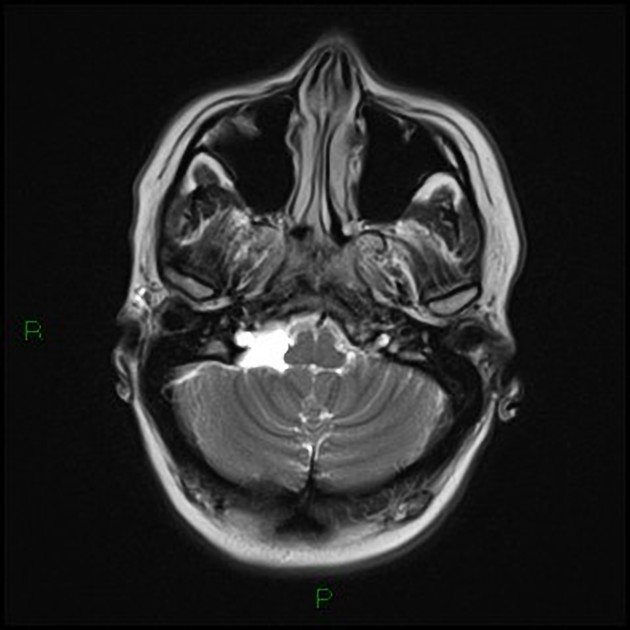
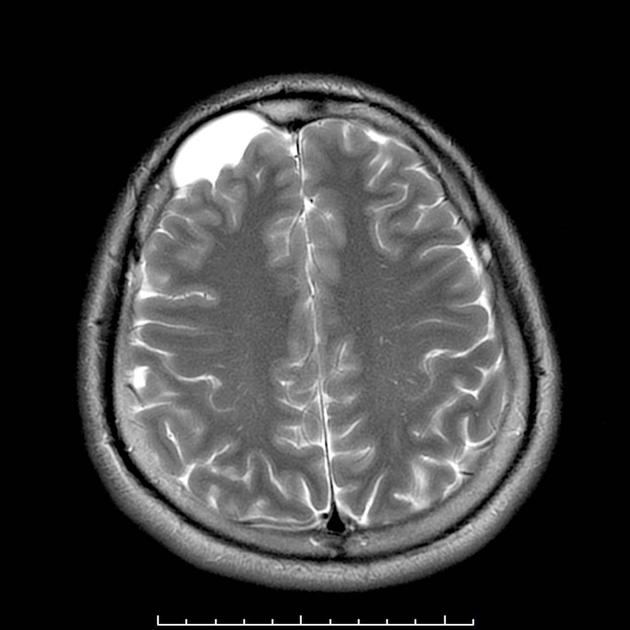
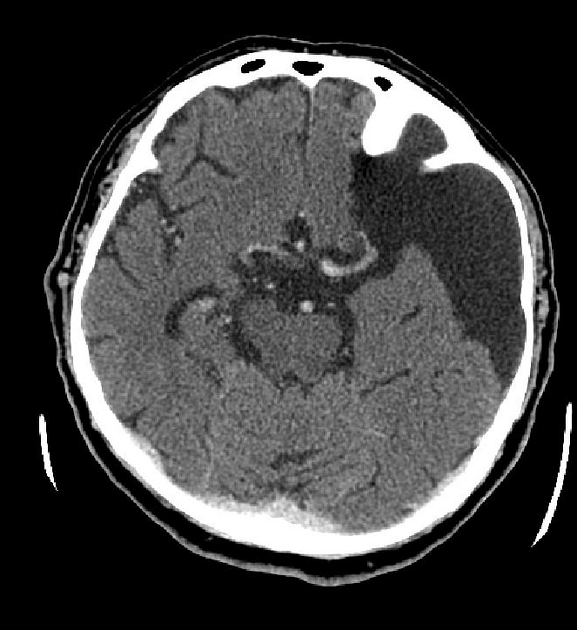
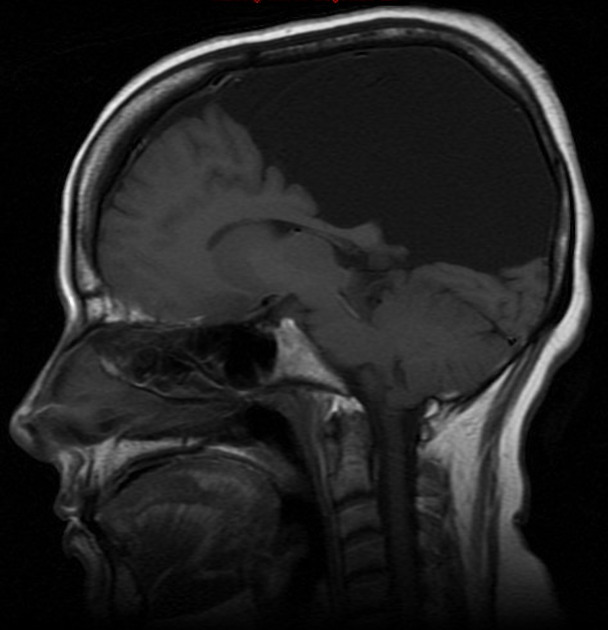
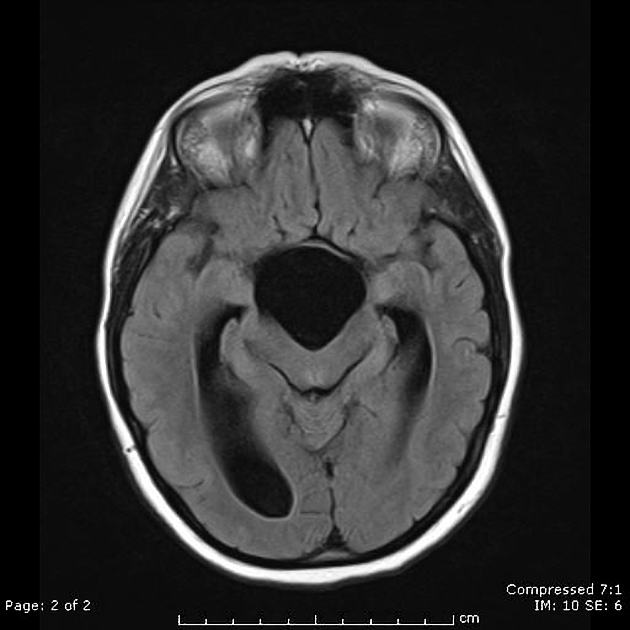
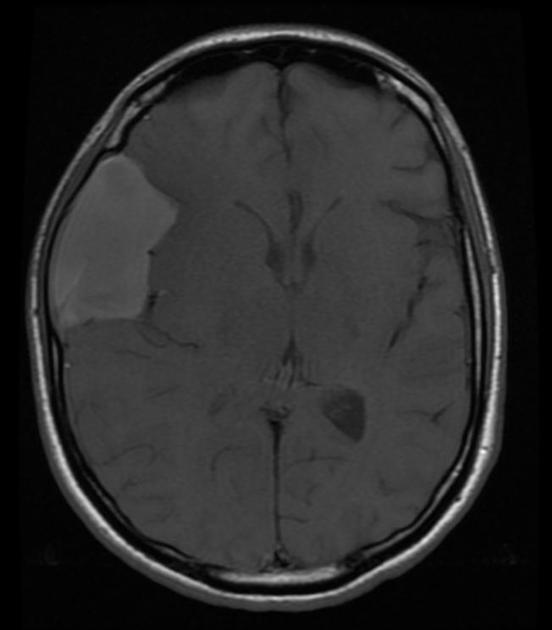
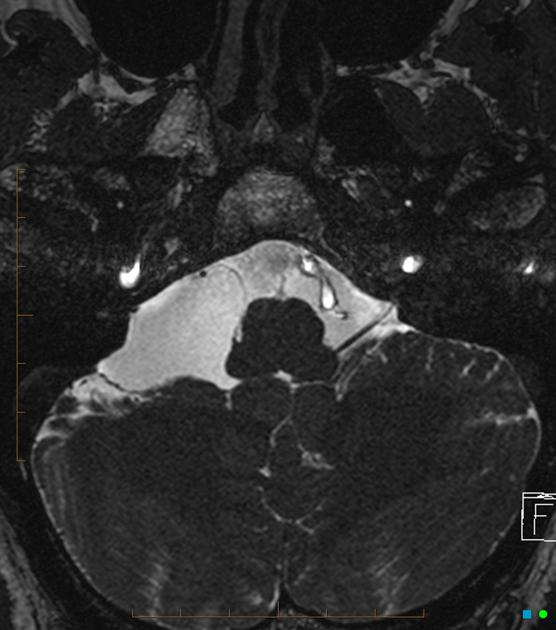
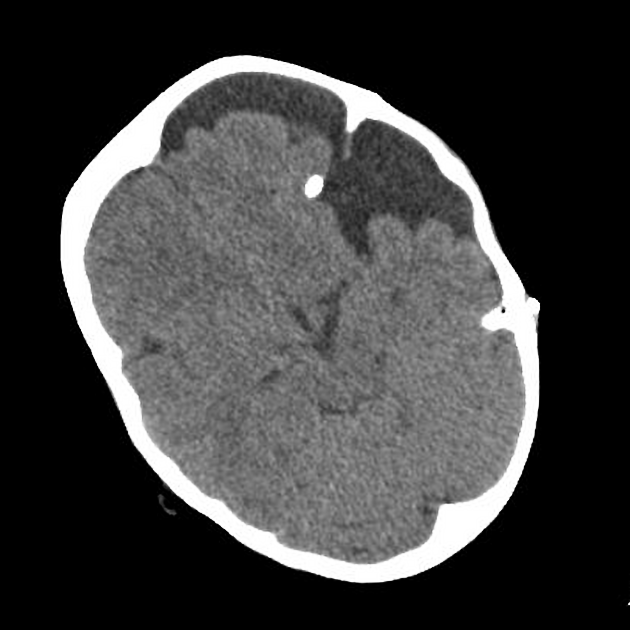
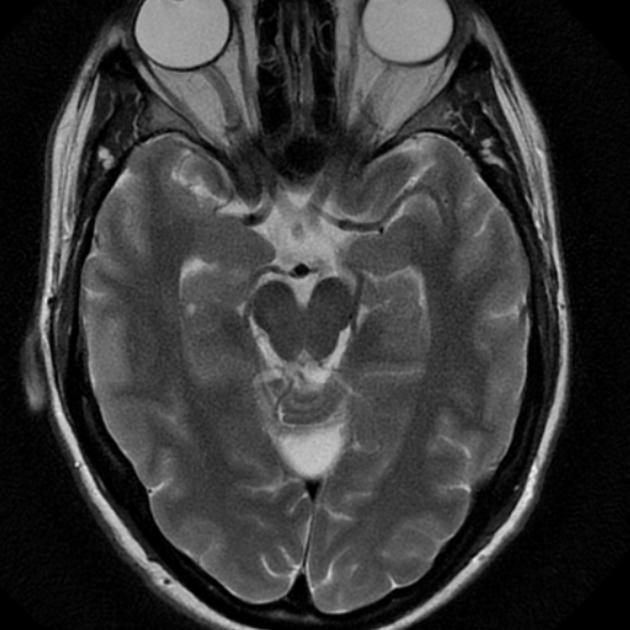
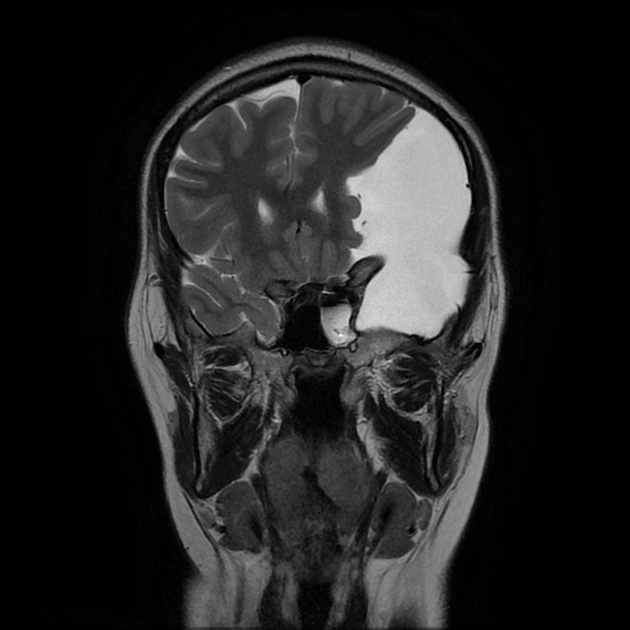
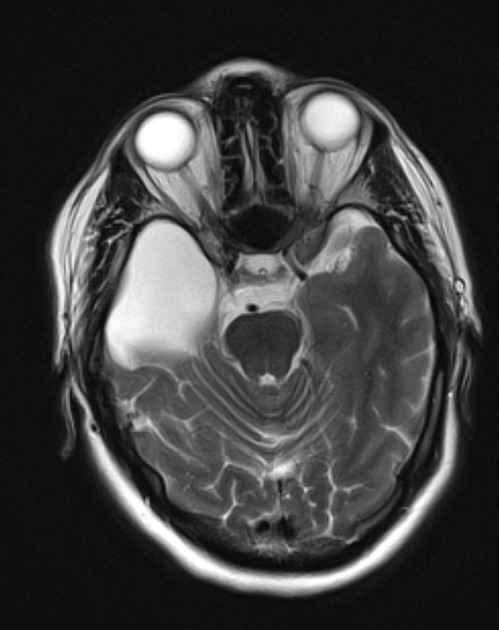
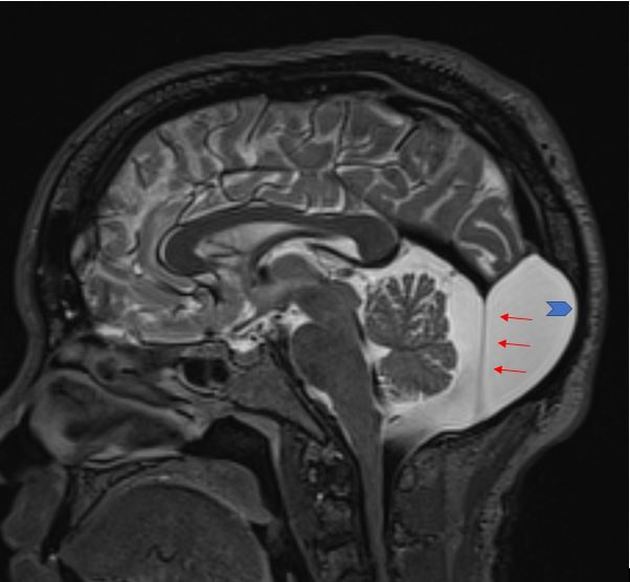
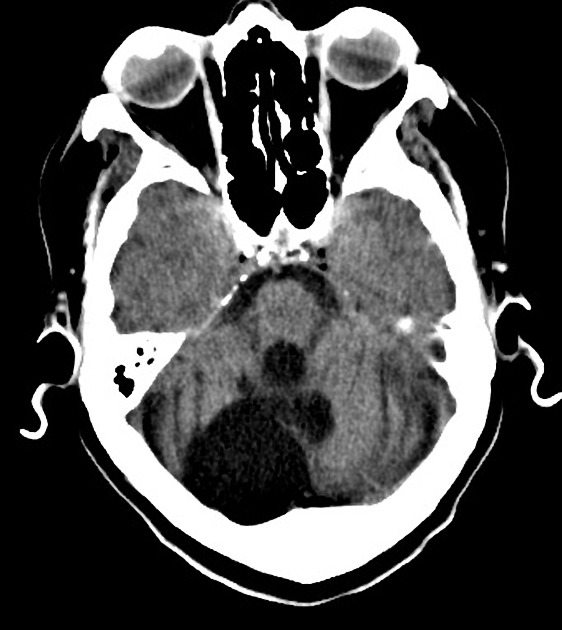
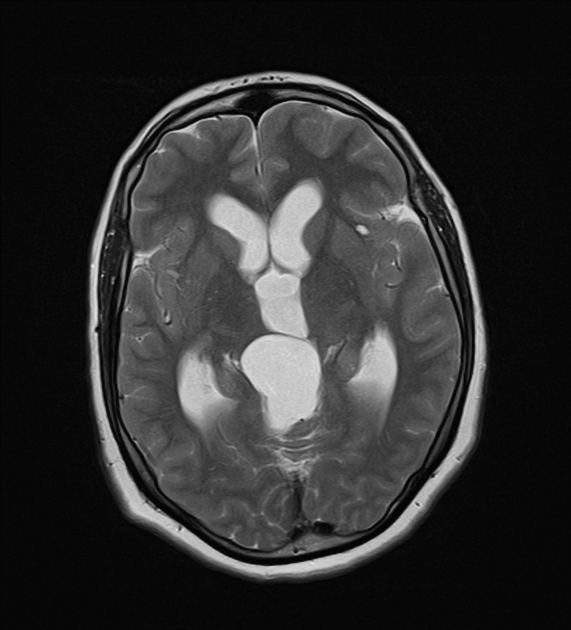
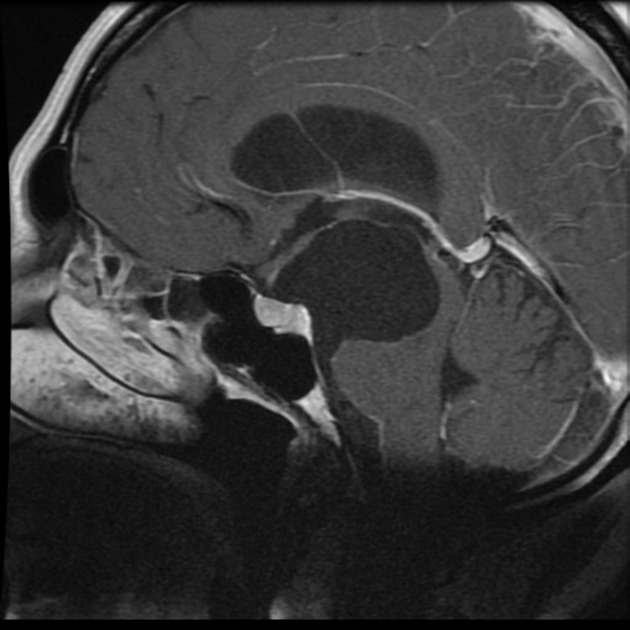
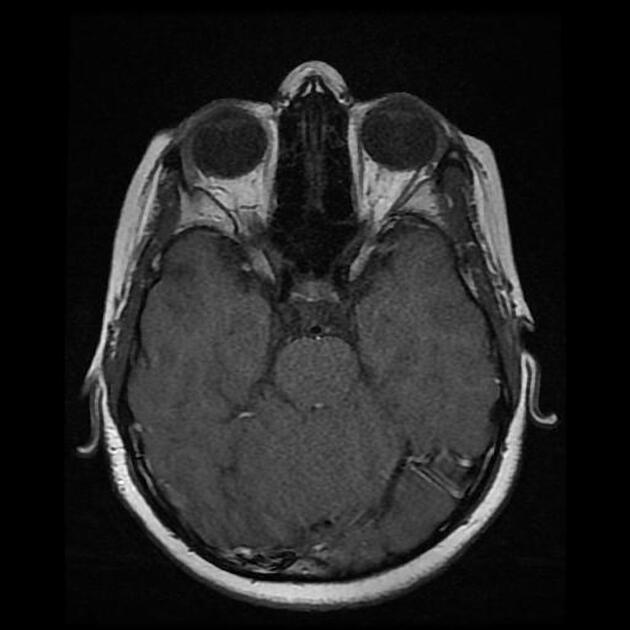
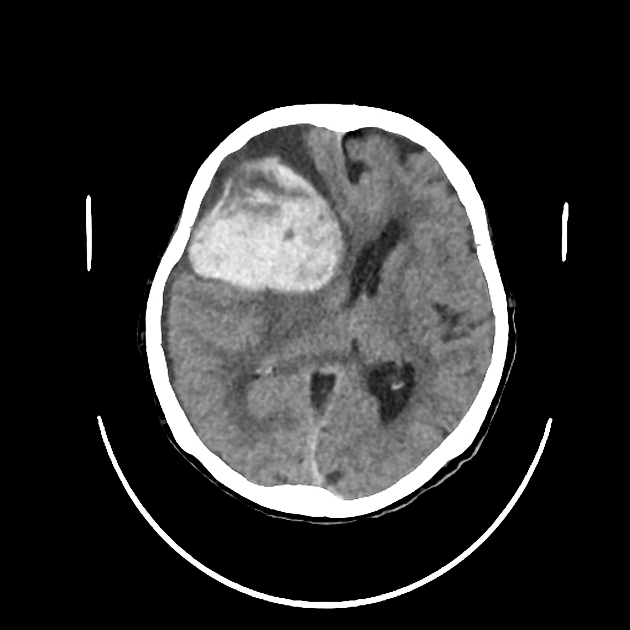
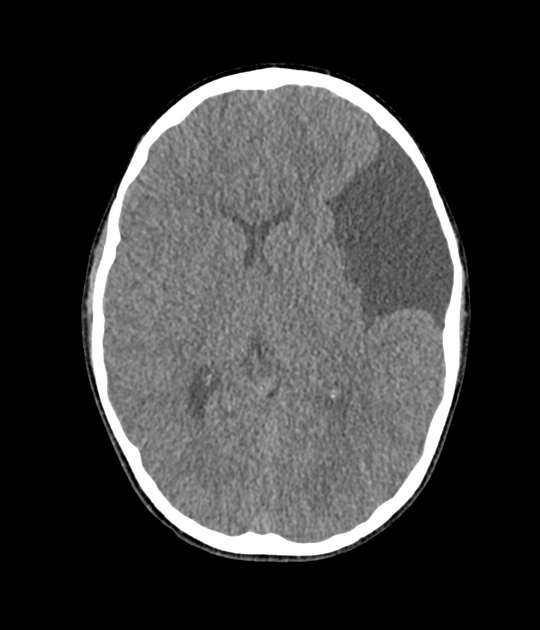
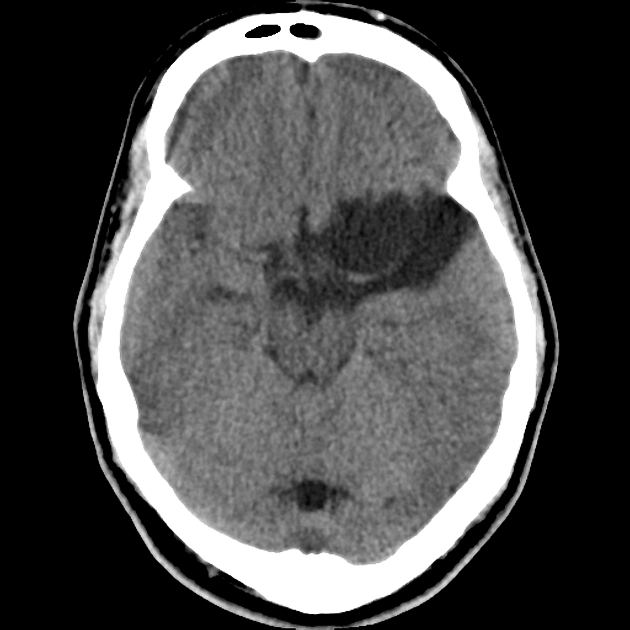
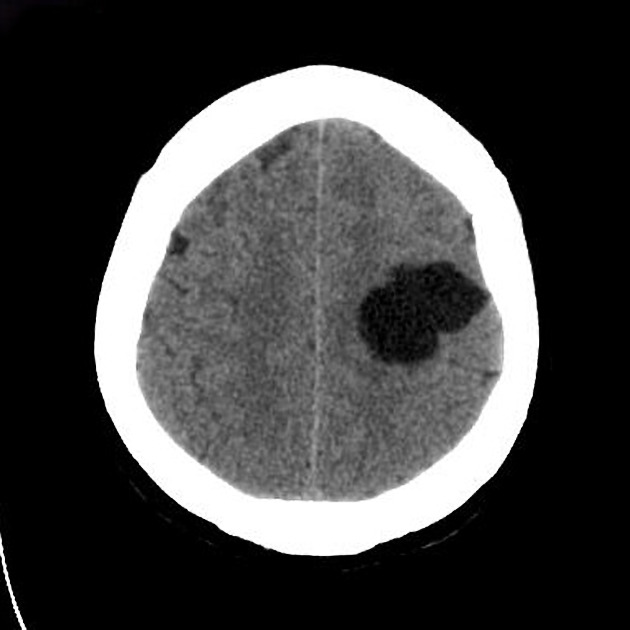
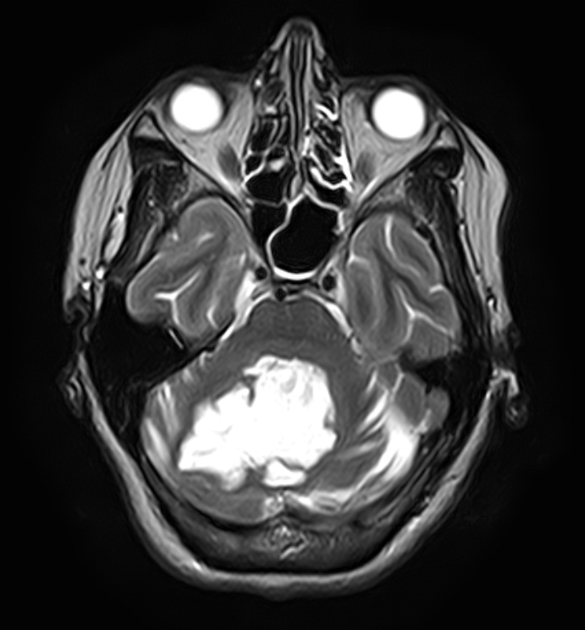
On imaging, they are characterised as well circumscribed cysts, with an imperceptible wall, displacing adjacent structures, and following CSF density on CT and CSF signal intensity on MRI (i.e. hyperintense on T2-weighted images with FLAIR suppression). They can have a remodelling effect on adjacent bone.
On this page:
Epidemiology
Arachnoid cysts account for ~1% of all intracranial masses. Although the vast majority are sporadic, they are seen with increased frequency in mucopolysaccharidoses (as are perivascular spaces).
In a retrospective cohort study of 48,417 patients who underwent neuroimaging, arachnoid cysts were identified in 661 patients (1.4%) with a statistically significant male predilection 4.
Clinical presentation
The majority of arachnoid cysts are small and asymptomatic. Approximately 5% of patients experience symptoms and when symptoms occur, they are usually the result of gradual enlargement resulting in mass effect 4. This results in either direct neurological dysfunction or distortion of normal CSF pathways resulting in obstructive hydrocephalus 3. Sellar/suprasellar, quadrigeminal, and cerebellopontine angle arachnoid cysts were more likely to be symptomatic 4.
Genetics
Arachnoid cysts are almost always sporadic and nonsyndromic, but association with acrocallosal, Aicardi, and Pallister-Hall syndromes have been reported 7.
In familial forms associated with lymphoedema-distichiasis syndrome, a mutation of the FOXC2 gene has been reported 8.
Pathology
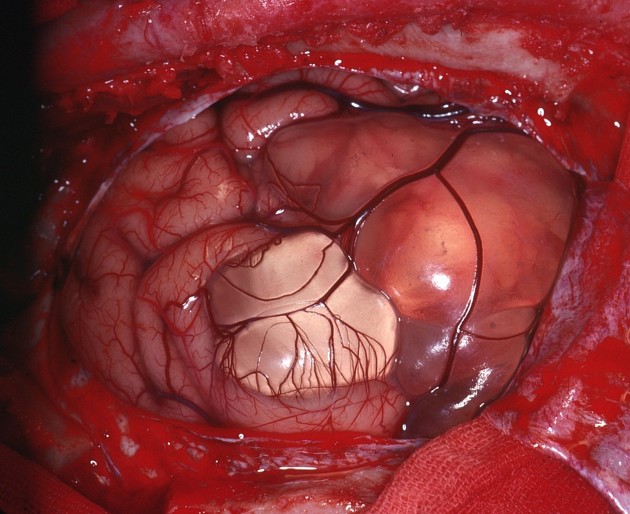
Arachnoid cysts are thought to arise due to congenital splitting of the arachnoid layer with accumulation of CSF within this potential space (thus technically they are intra-arachnoid cyst). The cyst wall is composed of flattened arachnoid cells forming a thin translucent membrane. There is no solid component and no epithelial lining.
Radiographic features
Arachnoid cysts can occur anywhere within the central nervous system, most frequently (50-60%) located in the middle cranial fossa, where they invaginate into and widen the Sylvian fissure. In this location, they can be classified into three types based on their size: see Galassi classification. Of these, Galassi type I is most common accounting for 78% followed by Galassi II and III with 19% and 3% respectively 4. The retrocerebellar location accounts for 30-40% of arachnoid cysts 4.
Some locations deserve special mention and separate discussion:
suprasellar cistern (see suprasellar arachnoid cyst)
within the ventricles (see intraventricular arachnoid cyst)
-
posterior fossa
cisterna magna (need to be distinguished from a mega cisterna magna)
cerebellopontine angle (need to be distinguished from an epidermoid cyst)
spinal canal (see spinal arachnoid cysts)
CT
Arachnoid cysts are extremely well circumscribed, with an imperceptible wall, and displace adjacent structures. When large, and over time, they can exert a remodelling effect on adjacent bone.
CT cisternography (introduction of contrast into the subarachnoid space) demonstrates communication of the cyst with the subarachnoid space. As this communication is slow, the cyst often fills later, and contrast may be seen to pool with it, outlining its dependent portion.
MRI
As they are filled with CSF, it is not surprising that they follow CSF on all sequences, including FLAIR and DWI. This enables them to be distinguished from epidermoid cysts, for example. As their wall is very thin, it only occasionally can be seen, and displacement of surrounding structures implies their presence. As there is no solid component, no enhancement can be identified.
Phase contrast imaging can also be employed, not only to determine if the cyst communicates with the subarachnoid space but to also identify the location of this communication.
Magnetic resonance cisternography: high resolution sequences such as CISS and FIESTA help delineate the cyst wall and adjacent anatomical structures.
Treatment and prognosis
Arachnoid cysts are benign, and the vast majority remain asymptomatic throughout life. If they are deemed to be causing symptoms, surgery can be contemplated. This can either take the form of a craniotomy (fenestration or excision) or placement of a cystoperitoneal shunt.
A rare complication is spontaneous rupture into the subdural space 6.
History and etymology
Richard Bright was the first to describe an arachnoid cyst in 1831 5.
Differential diagnosis
General imaging differential considerations include:
enlarged CSF space (e.g. mega cisterna magna)
-
often shows a heterogeneous/"dirty" signal on FLAIR
restricted diffusion
more lobulated
tend to engulf adjacent arteries and cranial nerves
leptomeningeal cyst: post-traumatic
-
subdural hygroma/chronic subdural haemorrhage
do not typically show CSF signal intensity on MRI
can have an enhancing membrane
-
cystic tumours: often will have a solid/enhancing component and be intra-axial
-
non-neoplastic cysts
-
often follow a history of trauma or stroke
surrounded by gliotic brain
tumefactive perivascular spaces, especially anterior temporal lobe perivascular spaces
-
small cyst
usually multiple when in the subarachnoid space






















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.