Atrial septal defect (ASD) is the second most common congenital heart defect after ventricular septal defect (VSD). Diagnosis is often delayed until adulthood when complications arise such as atrial arrhythmias or pulmonary hypertension. The radiologist may be the first to suggest the diagnosis by recognizing the typical features on a chest radiograph.
On this page:
Terminology
The term ASD is used loosely to describe any communication that allows blood to shunt between the atria in adults, including defects in the endocardial cushion, sinus venosus and coronary sinus.
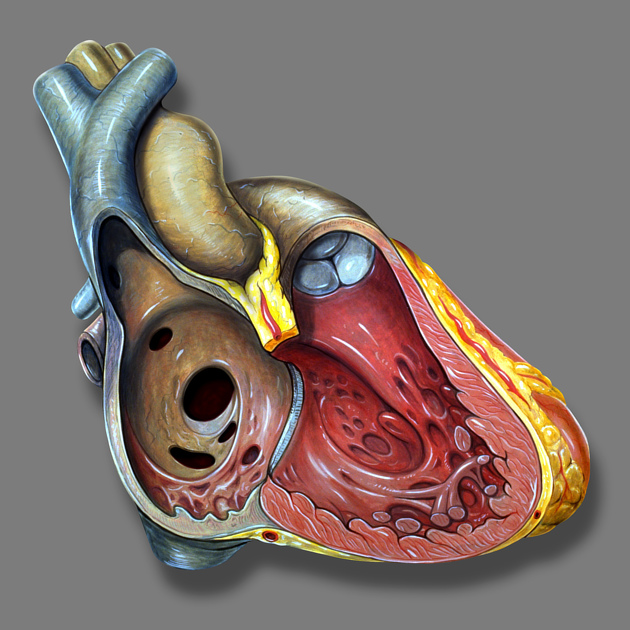
The true atrial septum is the small area around the fossa ovalis which could be removed without creating an epicardial fistula. The small size of this area of atrial contiguity is a consequence of the method of formation and the extent of the normal septum secundum. This septum results from the infolding of the atrial wall with associated epicardial tissues. The fossa ovalis is not covered by the septum secundum and the floor of the fossa is the embryologic septum primum.
Although defects in the true septum are commonly known as ‘secundum ASDs’ they could also be described as fossa ovalis defects. ‘Secundum defect’ most likely refers to the normal absence of septum secundum in this area however a pathological ASD requires that the fossa ovalis is not closed by the underlying septum primum which can be due to malformation of one or both of these structures.
Secundum ASD is often confusingly taken to refer to the ostium secundum, the normal hole that develops in the septum primum close to the atrial roof. In the fetus, this is connected to the fossa ovalis forming the channel which allows right-to-left shunting to continue after the ostium primum closes (when the septum primum fuses with the endocardial cushions). At autopsy, in up to 34% of adults, this connection persists as a probe-patent tunnel running from the fossa ovalis to the ostium secundum, and this has been labeled ‘patent foramen ovale’ 15, 16, 21.
Epidemiology
Atrial septal defects account for 10% of congenital heart disease and are more common in women, M:F = 1:2. Close family history of ASD was found in 2%.
Associations
Atrial septal defects are seen in association with the following:
Down syndrome 19: 50% have congenital heart disease and endocardial cushion defects predominate, outnumbering secundum ASD
other trisomies
Holt-Oram syndrome: autosomal dominant inheritance, mutations of the T-box-5 gene (TBX5) prevent normal development of the upper limbs and heart
Ellis-van Creveld syndrome (chondroecterdermal dysplasia): 50% have mutations in the EVC or EVC2 genes, autosomal recessive inheritance, rare but more prevalent in Old Order Pennsylvanian Amish and Western Australian Indigenous peoples
familial ASD (without skeletal manifestations), autosomal dominant due to mutations in the cardiac transcription factor NKX2.5
GATA4 gene variants also have a role in ASD
Clinical presentation
All patients with the above syndromes are best evaluated with ultrasound. Non-syndromic ASD is typically clinically occult (in contrast with small transitory VSDs where the high-pressure difference generates a loud noise and even a palpable thrill). There are typically no symptoms and subtle flow-related signs, such as fixed wide splitting of the second heart sound or a pulmonary flow murmur. In larger shunts, exercise intolerance, exertional dyspnea, and recurrent pneumonia may occur.
Even with good healthcare, more than 50% do not present until adulthood and the onset of complications such as atrial fibrillation, pulmonary hypertension, and right heart failure. Left ventricular compliance decreases with age, causing increased left-to-right shunting. By the age of 60 years, almost all will be symptomatic ref.
ECG
Uncomplicated secundum ASD:
sinus rhythm
right axis deviation
rSR’ trace in V1
right bundle branch block (indicates dilated RVOT)
Ostium primum ASD:
prolonged PR interval (due to left atrial dilatation)
left axis deviation
rSR’ trace in V1
right bundle branch block or interventricular conduction delay
Sinus venosus defect:
negative P wave in lead III
left axis deviation
Pulmonary hypertension affects these findings in the following ways:
loss of rSR’ trace in V1
tall monophasic R wave and deep inversion of the T wave
Finally, a ‘crochetage’ notch in the terminal upstroke of the the R wave in the inferior limb leads has been reported as a marker of secundum ASD which correlates with the size of the shunt 10
Pathology
Embryology
(For a full description see development of the heart.)
The fetal circulation must bypass the developing lungs until birth when they take on their role in respiration. The pulmonary vasculature is now sufficiently developed to function in series with the systemic circulation.
Division of the atrial chambers begins as the thin septum primum grows from the atrial roof towards the endocardial cushions at the atrioventricular junction. The ostium primum is the gap between the septum and the cushions. Before the ostium primum closes, the ostium secundum must open, which lies near the atrial roof.
The septum secundum forms by incomplete invagination of the atrial wall along the right atrial aspect of the septum primum leaving a bare area of septum primum at the fossa ovalis. Blood continues to shunt from right to left through the patent foramen ovale, exiting through the ostium secundum. After birth and the onset of respiration, the left atrial pressure rises. This pushes the septum primum against the fossa ovalis (like a flap valve) causing functional closure. In about 2 out of 3 people adherence closes the tunnel over the ensuing months 15.
Types
There are four main types of defect commonly included, however, only the first two and PFO are true septal defects:
-
secundum ASD (fossa ovalis) 15,20
the fossa ovalis may be large or the septum primum deficient
75% of all ASDs, 7% of congenital heart defects rising to 40% after 40 years of age
usually an isolated abnormality
-
primum ASD (endocardial cushion defect)
15-20% of ASDs
a spectrum from primum ASD with cleft mitral valve to atrioventricular septal defect with common AV valve (AV canal) 17
strong association with trisomy 21
50% mortality within 1 year if untreated
-
sinus venosus defects
<10%
superior is much more common and is typically associated with anomalous drainage of the right superior pulmonary vein into the SVC
inferior defect is typically associated with anomalous drainage of the right inferior pulmonary vein into the IVC
-
<1%
coronary sinus drains to the left atrium
associated with persistent left SVC
A patent foramen ovale (PFO) is a persistent small tunnel from the fossa ovalis to the fetal ostium secundum. They can be a source of paradoxical emboli when right atrial pressure is elevated (e.g. Valsalva maneuver, pulmonary hypertension). In one autopsy series, 34% probe patency was established.
Radiographic features
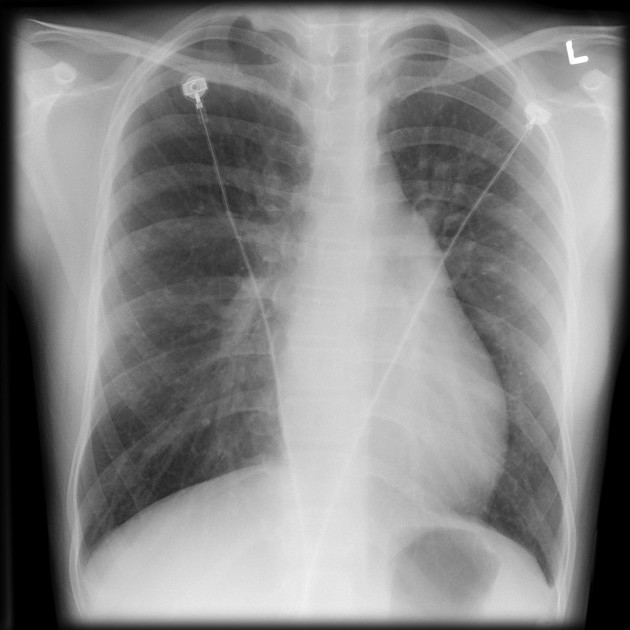
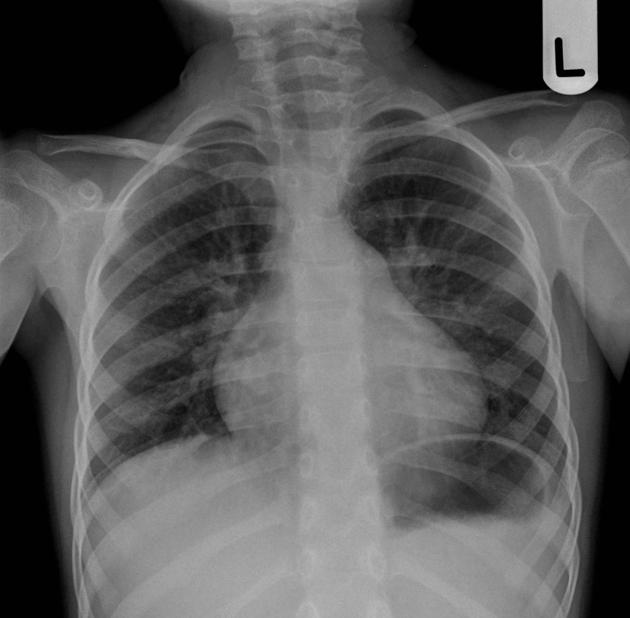
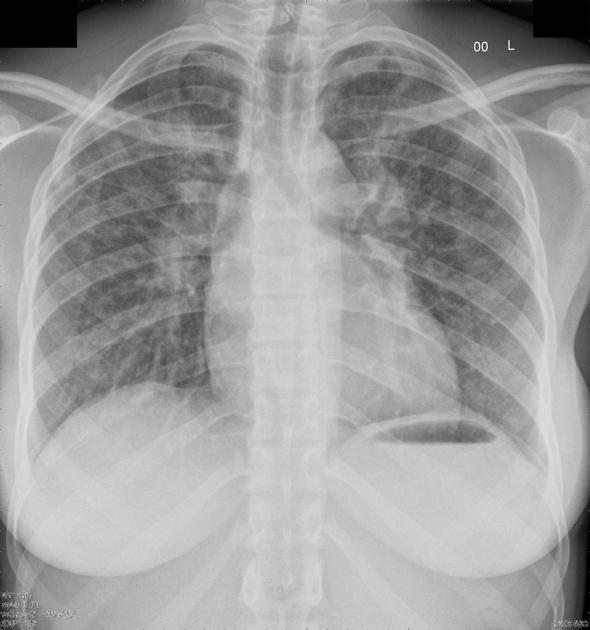
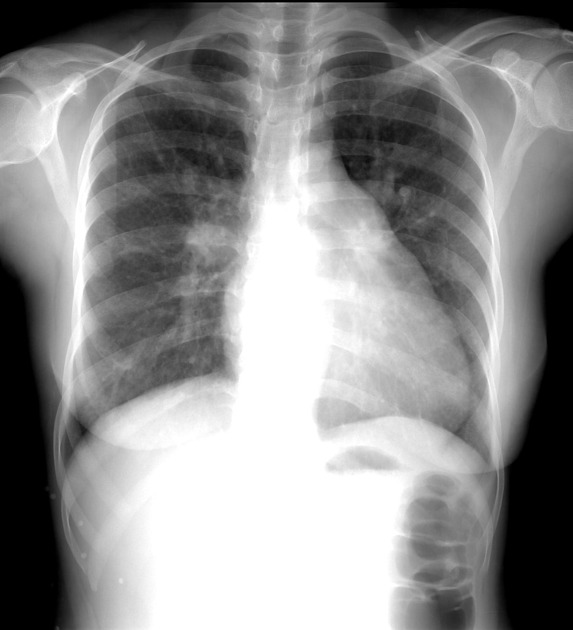
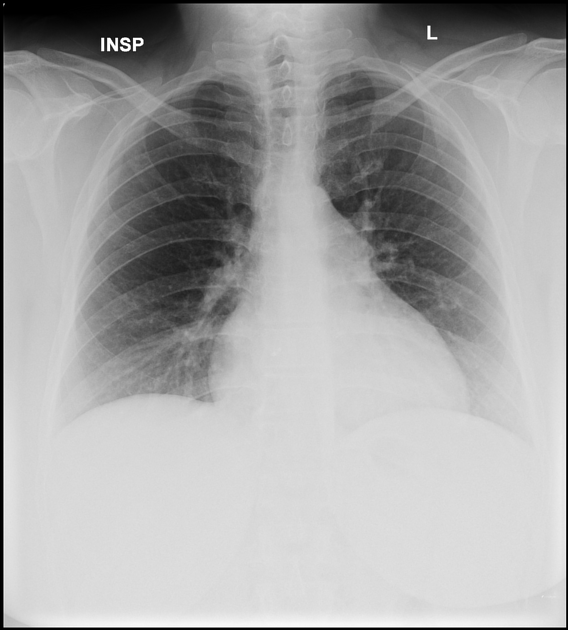
Plain radiograph
Appearances depend on the shunt size, the presence or absence of mitral incompetence and the age of the patient:
normal when the atrial septal defect is small and there are no complications
-
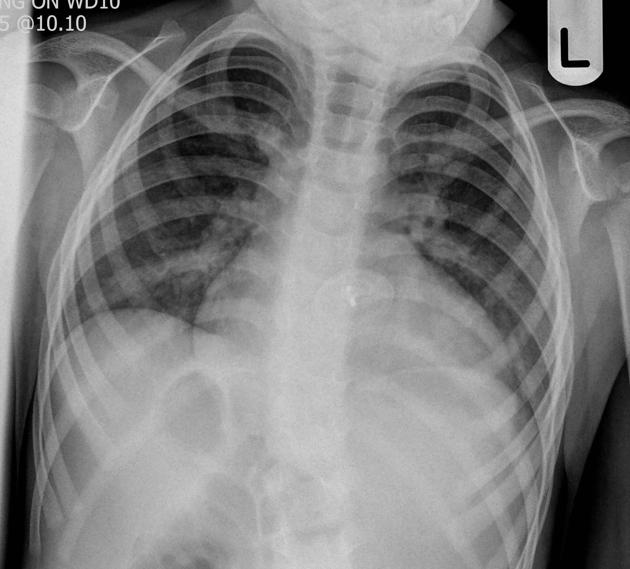
plaeonaemia (pulmonary plethora) due to increased pulmonary blood flow
enlarged pulmonary vessels throughout the lungs
vessels visible to the periphery of the lung
cardiomegaly due to right atrial and right ventricular dilatation
-
pulmonary hypertension
dilated proximal pulmonary arteries
peripheral (arterial) pruning
right ventricular hypertrophy (upturned apex, broad area of sternal contact on lateral view)
small normal aortic knuckle
left atrial dilatation only occurs if there is mitral incompetence
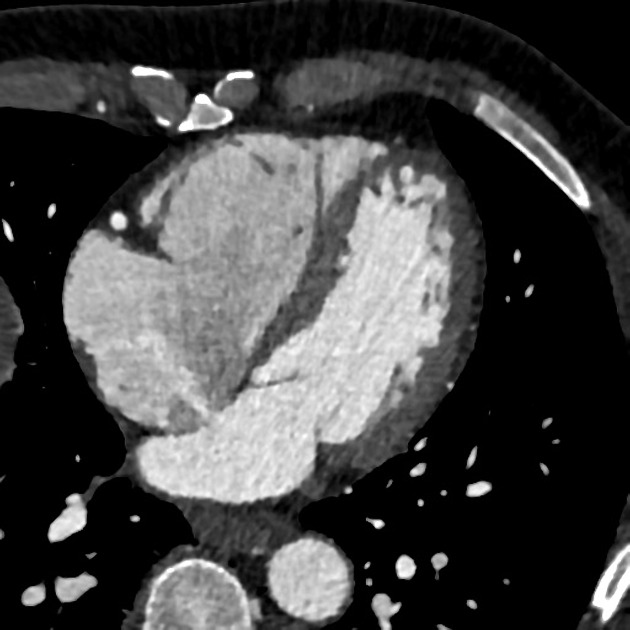
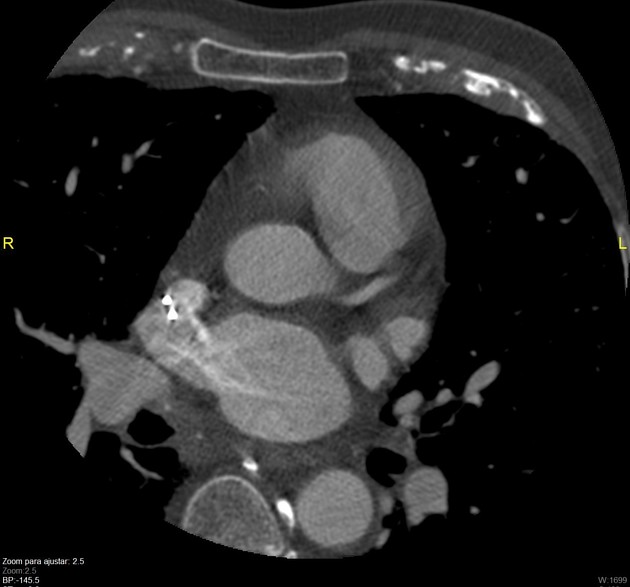
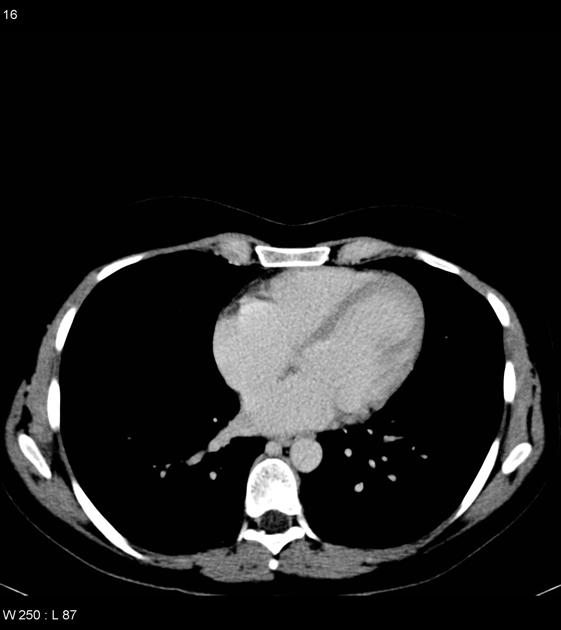
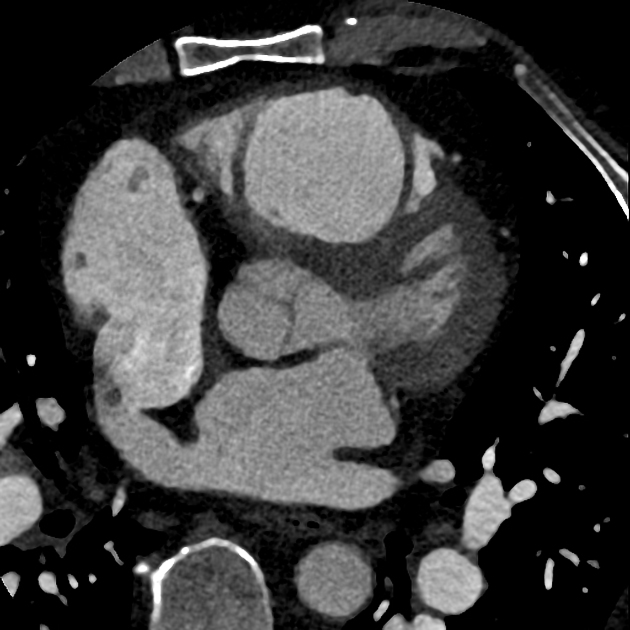
CT
The same features are better delineated compared with an x-ray and chamber diameter, wall-thickness and aorto: pulmonary ratio can be assessed. (The cardiac phase can be estimated if the contrast medium outlines the valves.) The defect may be shown. In the case of a sinus venosus defect, PAPVR is likely to be present. PFO may be seen if a saline chaser is given; a small jet of opacified blood may extend obliquely through the septum to the roof of the left atrium 20. Unroofed coronary sinus drains to the left atrium and can be associated with persistent SVC. Coronary artery assessment is useful in older patients ref.
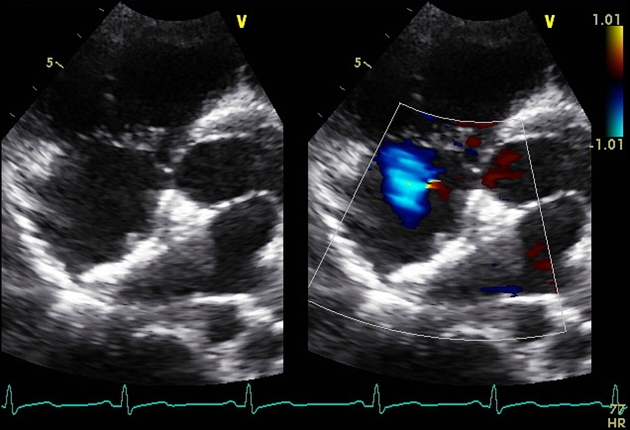
Ultrasound
The defect may be seen and measured although sinus venosus defects may only be seen on TOE ref. Tricuspid regurgitation is more frequent when the right heart chambers are dilated and allow an estimate of right ventricular pressure ref.
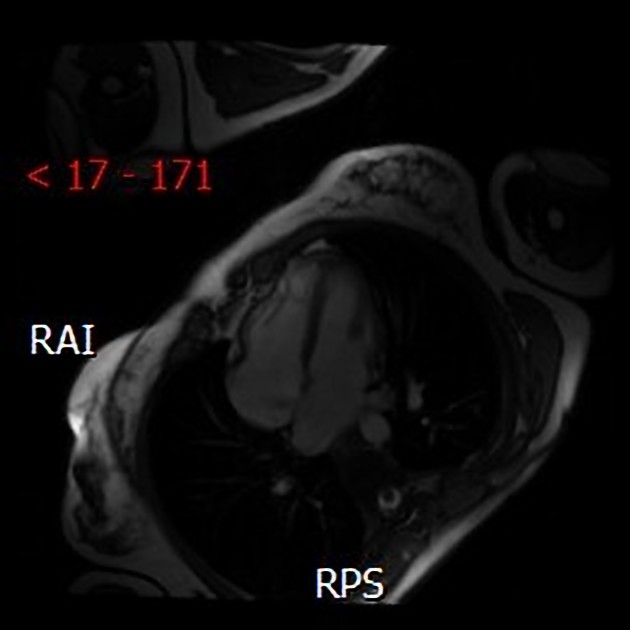
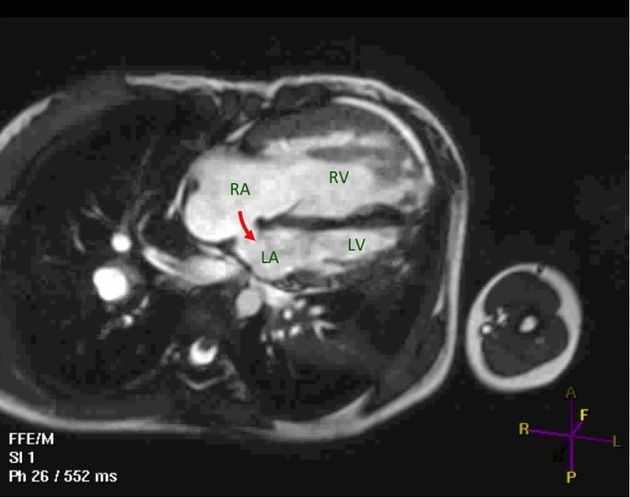
MRI
Used for structural and functional assessment as well as shunt quantification by measuring the ratio of pulmonary blood flow (Qp) to systemic blood flow (Qs), i.e. Qp:Qs 18.
Angiography (DSA)
Coronary catheterization may be useful if pressure measurements were not reliable or for coronary artery assessment in older patients ref.
Treatment and prognosis
Complete AV canal has a 50% mortality if uncorrected during the first year of life. In contrast, small ASDs may close in childhood and others may not present until the age of 60! Overall, survival is <50% beyond age 40-50 years and subsequent death rate is about 6% per annum.
Ultrasound assessment demonstrates which defects are suitable for trans-catheter closure by device and helps guide the procedure. Cardiac perforation can complicate the procedure.
Some defects require surgery and this carries a mortality rate of <3%.
Both surgery and device placement carry a risk of atrial arrhythmias and thromboembolism.
Complications
if pulmonary hypertension has developed, pregnancy is high risk due to increased circulating volume and increased cardiac output 14
atrial arrhythmias e.g. atrial fibrillation
pulmonary hypertension leading to Eisenmenger syndrome and right heart failure
-
mitral valve prolapse due to altered geometry 17













 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.