Bowel perforation, either small bowel perforation or large bowel perforation, can occur in many different settings, but the more common are
bowel obstruction (both small and large)
severe ulcer disease
diverticular disease
infection
-
malignant diseases
gastrointestinal tumors
direct tumor invasion
trauma: blunt or penetrating
autoimmune
iatrogenic e.g. perioperative, endoscopy
Esophageal perforation is technically a bowel perforation, but the causes, evaluation, and prognosis differ, so it is covered in its section.
Bowel perforation in neonates is often due to necrotizing enterocolitis and is covered separately.
On this page:
Clinical presentation
The classic presentation is sudden and severe abdominal pain, sometimes with localized peritonism or a rigid abdomen on examination.
The presentation may change depending on the etiology, however. If the perforation is due to bowel obstruction, for instance, there may be an initial relief of pain as the dilated bowel collapses. Then the pain begins again when peritonitis develops.
Radiographic features
The imaging diagnosis of bowel perforation almost always relies on seeing pneumoperitoneum 2.
Plain radiograph
free gas under the diaphragm is a classic sign of pneumoperitoneum on the erect chest and abdomen radiographs and it is suspicious for bowel perforation
other signs of pneumoperitoneum, including Rigler sign
Fluoroscopy
-
suspected gastroduodenal perforation
an upper GI study with water-soluble contrast medium is not usually the primary study for detection of a suspected gastric or duodenal perforation but can be useful for confirmation of an equivocal appearance on CT or for detection of the precise location of a small perforation
-
suspected small bowel perforation
small bowel follow-through is inferior to CT of the abdomen and pelvis with oral contrast for detection and localization of small bowel perforation
-
suspected colonic perforation
-
a single contrast barium enema is not usually appropriate in the setting of colonic perforation
the reason for colonic perforation is usually apparent and these patient are usually operated upon emergently
-
Ultrasound
although not a primary modality for evaluating pneumoperitoneum, free gas can be detected on ultrasound when gas shadowing is present along the peritoneum 4
make sure that the gas is not within the colon before deciding on calling pneumoperitoneum
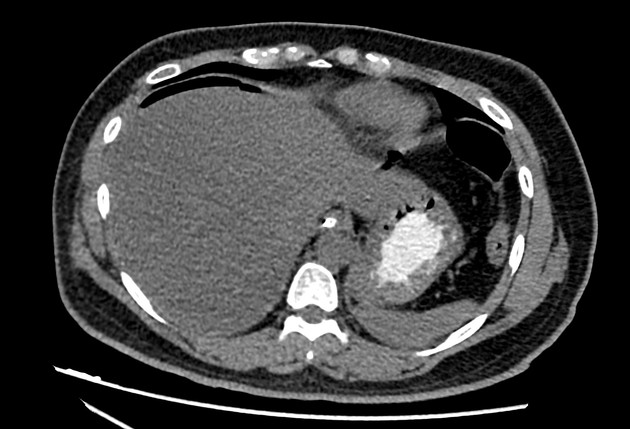
CT
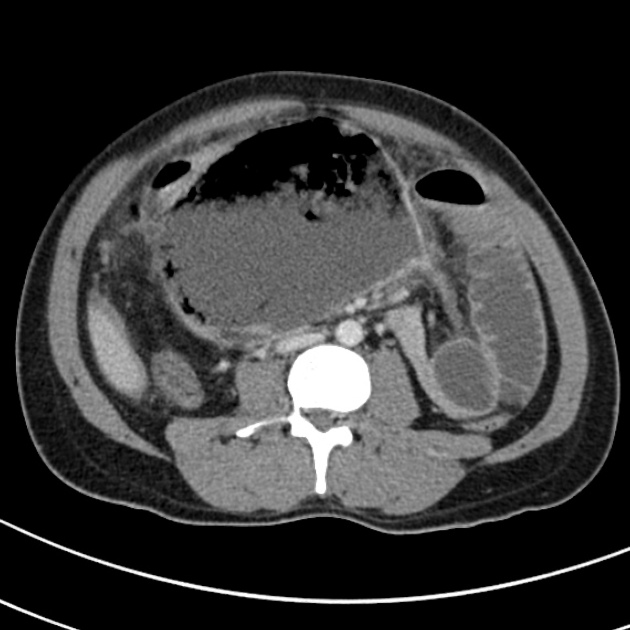
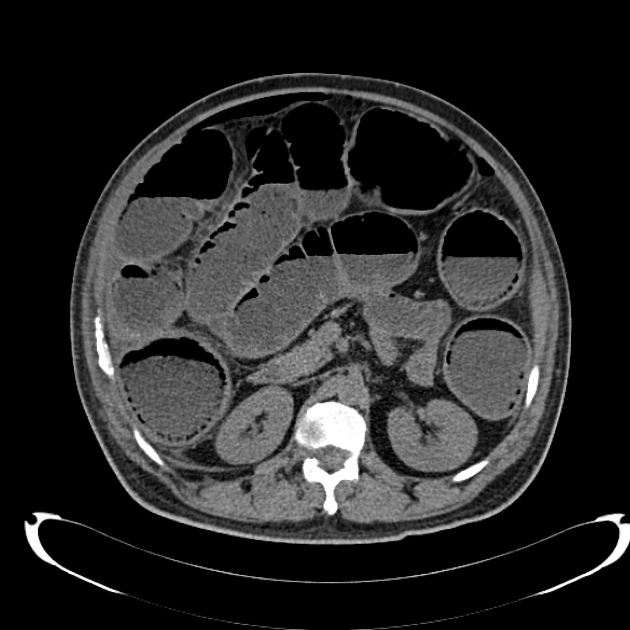
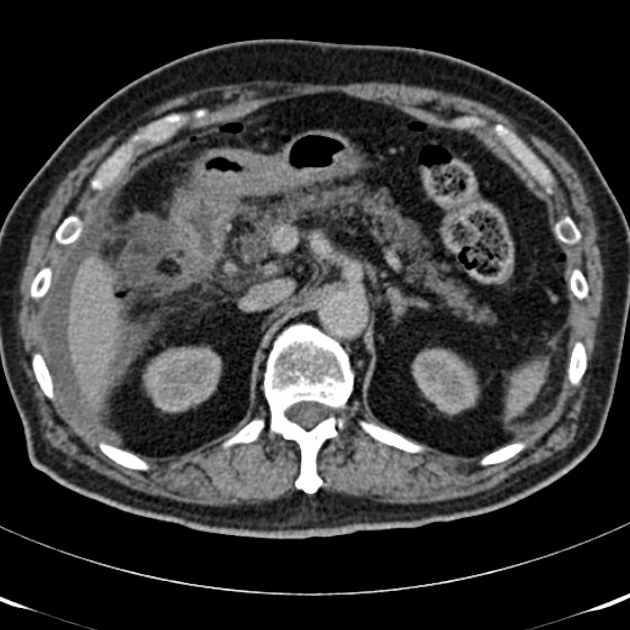
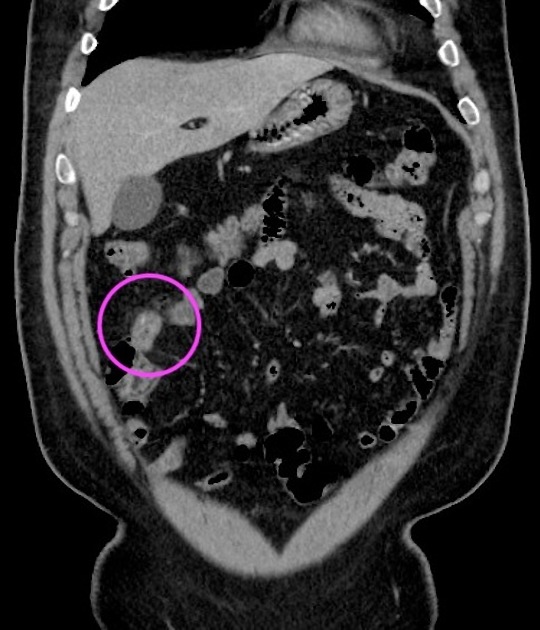
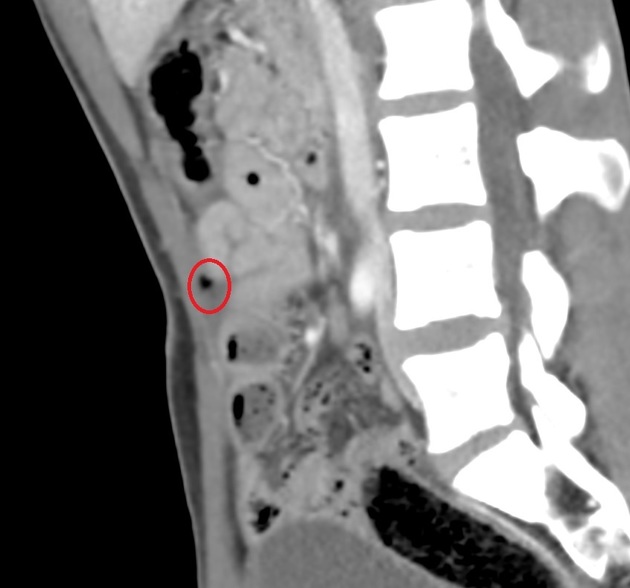
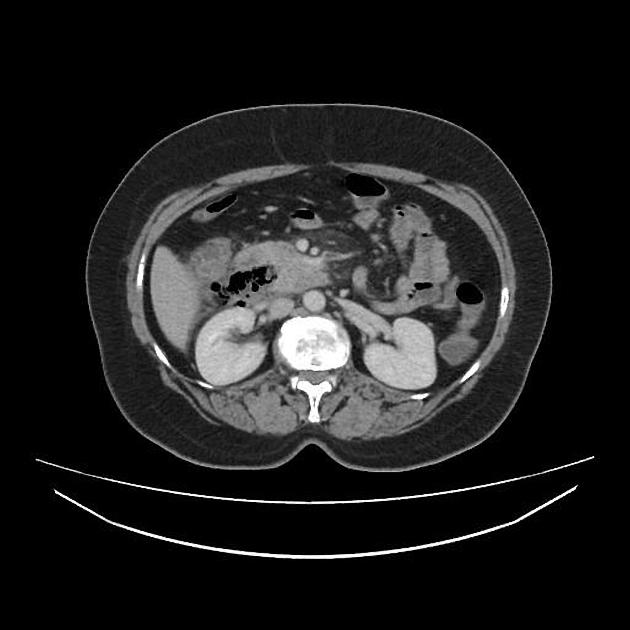
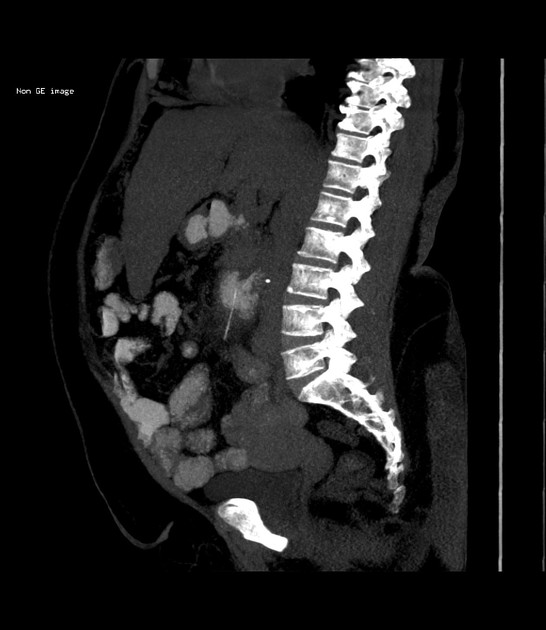
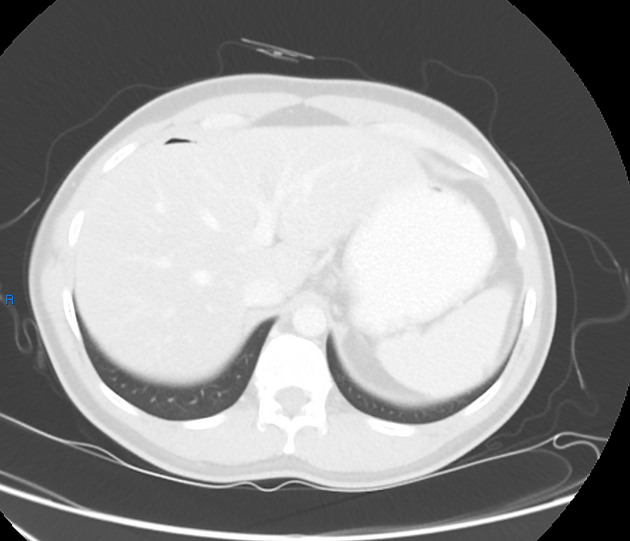
CT is the primary imaging modality for detection and localization of bowel perforation. CT is accurate in detecting the site of perforation in 85% of the cases 1. The site of the perforation can often be localized by:
tracking pneumoperitoneum toward a region of bowel: if gas is in the upper abdomen, upper GI perforation is more likely, meanwhile, if gas is found within the pelvis, perforation is more likely to be colon or less frequently, small bowel 1; if gas is extraperitoneal, the perforation site is likely to be retroperitoneal 1
localized peritoneal fat stranding, bowel wall thickening, or abnormal bowel wall enhancement 1
bowel wall discontinuity 1
-
oral contrast leak (if administrated) 1
if a suspected bowel perforation is the primary indication for the study, then protocolling the study with a water-soluble contrast medium is useful ref
if a bowel perforation occurs due to obstruction, the perforation usually occurs at the site of maximal bowel distention and the perforation may be distant from the actual cause of the bowel obstruction ref
bowel perforation may not result in pneumoperitoneum, but liquid contents exiting the bowel may form a phlegmon or abscess ref
Treatment and prognosis
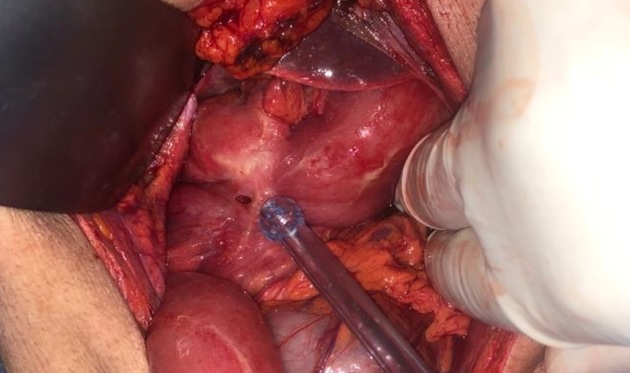
Because spillage of bowel contents into the peritoneal space can result in fatal peritonitis, these patients have traditionally received immediate operative treatment.
Some non-septic patients may not need immediate surgery if the perforation is small or contained, and instead can be covered with antibiotic therapy 5.
Differential diagnosis
-
in the absence of a definitive point of luminal contrast leak, differential considerations are primarily those for pneumoperitoneum
recent surgery
peritoneal drains or dialysis catheters
increased airway pressure for ventilation
Practical points
colonic perforation tends to result in a greater amount of pneumoperitoneum than free fluid
upper GI perforation tends to present with a relatively large volume of free fluid and less pneumoperitoneum
the presence of pneumoperitoneum in the periportal region is also suggestive of upper GI perforation 6











 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.