This is a basic article for medical students and other non-radiologists
Cerebral abscesses represent focal areas of infection within brain parenchyma, usually containing pus and having a thick capsule. They typically have enhancing walls and can mimic a number of other significant pathologies.
On this page:
Reference article
This is a summary article; read more in our article on cerebral abscess.
Summary
-
epidemiology
- may occur at any age
- risk factors
- immunocompromise (including HIV, diabetes mellitus)
- existing infection (eg. middle ear infection, bacteremia)
- IVDU
-
presentation
- fever, headache, and focal neurology may be present
- signs of raised ICP, focal neurology or seizures should prompt imaging
-
pathophysiology
- spread of infection to the brain
- inflammation and irritation of parenchyma
- thin walled abscess formation
- inflammation and irritation of parenchyma
- source
- hematogenous spread is the commonest route 1
- infection crosses the blood-brain barrier
- direct infection may occur
- mastoiditis or sinusitis
- requires a severe infection and bone destruction
- hematogenous spread is the commonest route 1
- microbiology
- mixed bacteriology
- sterile cultures in 25-34% of cases 1,2
- gram negative bacteria commoner in pediatrics and immunocompromised patients
- fungal infection commoner in the immunocompromised
- spread of infection to the brain
-
investigation
- blood work to include inflammatory markers and renal function
- cross-sectional imaging
- CT with contrast - first line
- MRI (diffusion-weighted imaging is important)
-
treatment
- usually require operative management
- aggresive IV antibiotic therapy 1
Imaging
-
role of imaging
- initial diagnosis
- assessment of any mass-effect, e.g. from surrounding edema
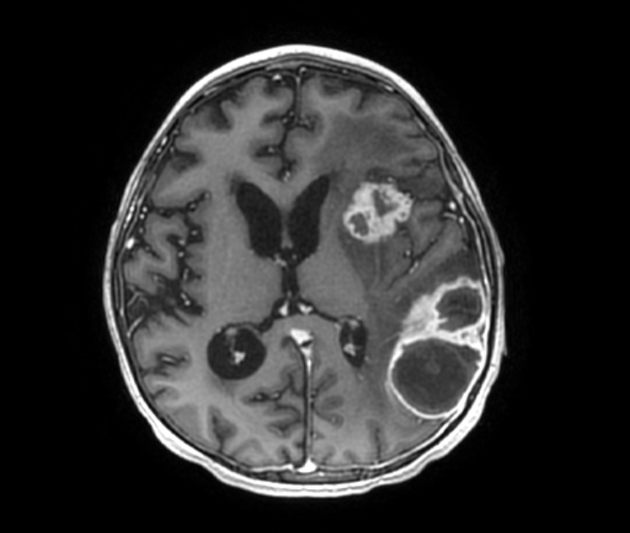
- assessment of any other lesions
- aid surgical planning
-
radiographic features
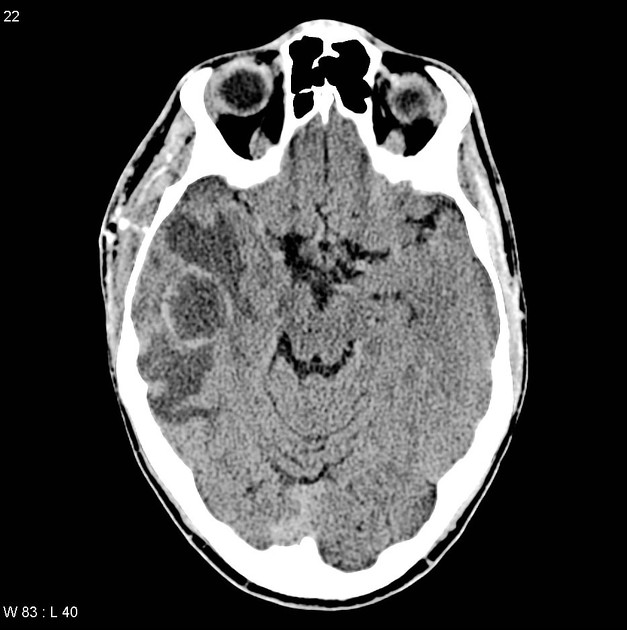
- CT
- first line imaging
- low-density lesion with peripheral enhancement
- surrounding low-density white-matter edema
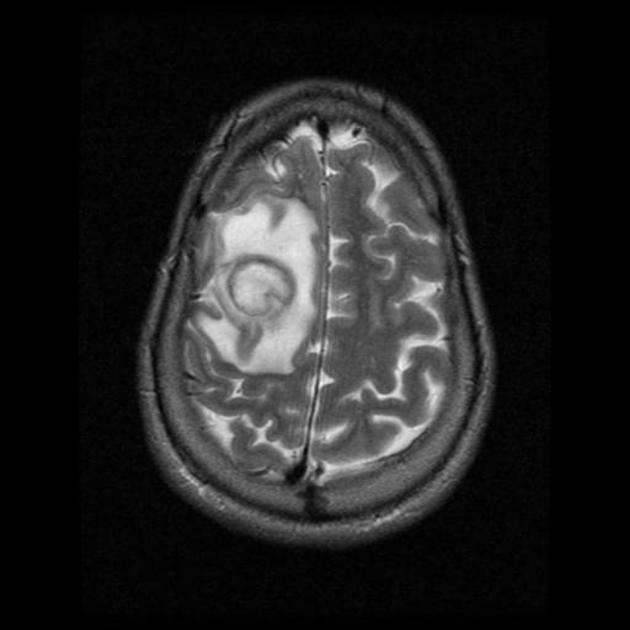
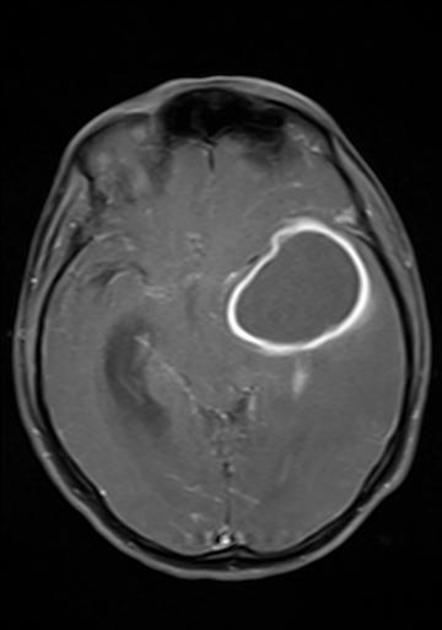
- MRI
- more sensitive
- pus is bright on T2 weighted images
- the wall of the abscess typically enhances post contrast
- diffusion restriction within the abscess cavity is helpful to make the diagnosis
- CT





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.