Choroid plexus papillomas are an uncommon, benign (WHO grade 1) neuroepithelial intraventricular tumour, which can occur in both the paediatric (more common) and adult population.
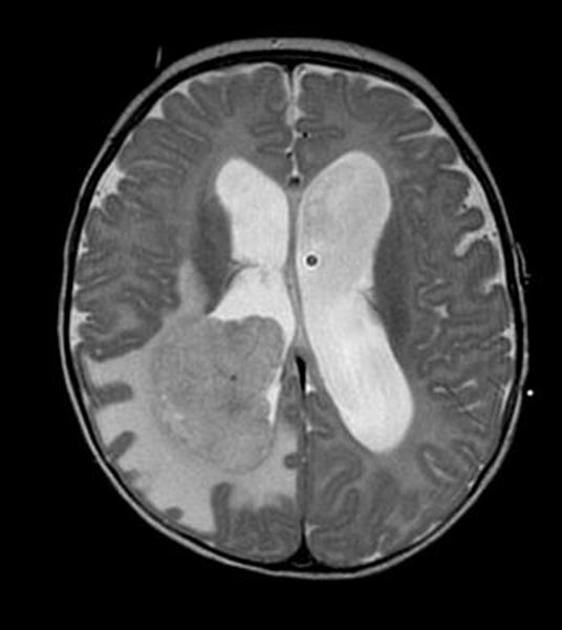
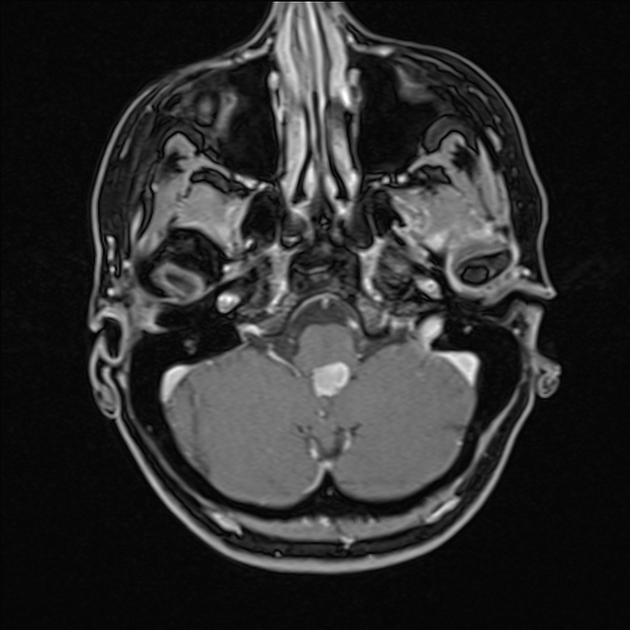
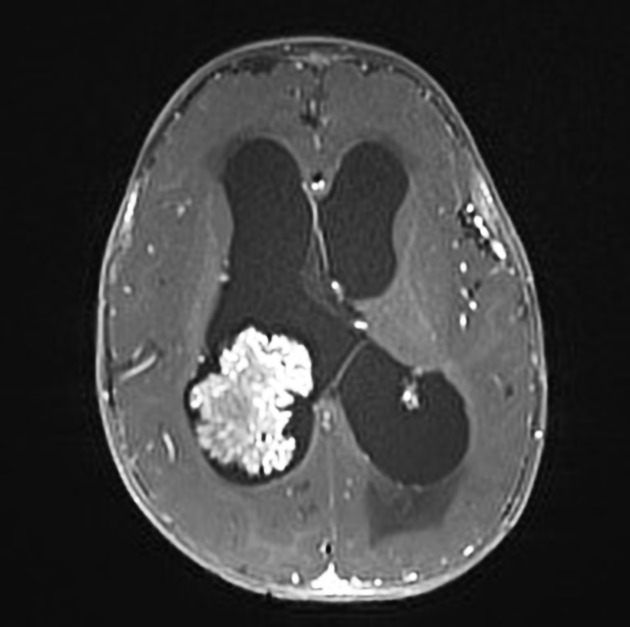
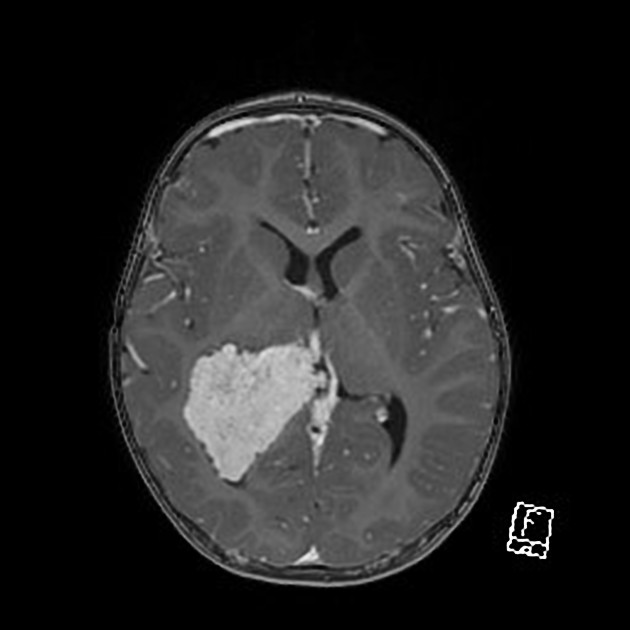
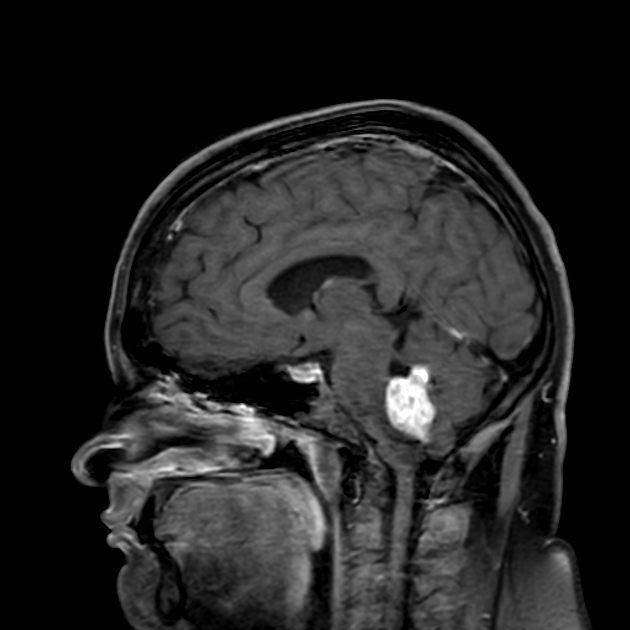
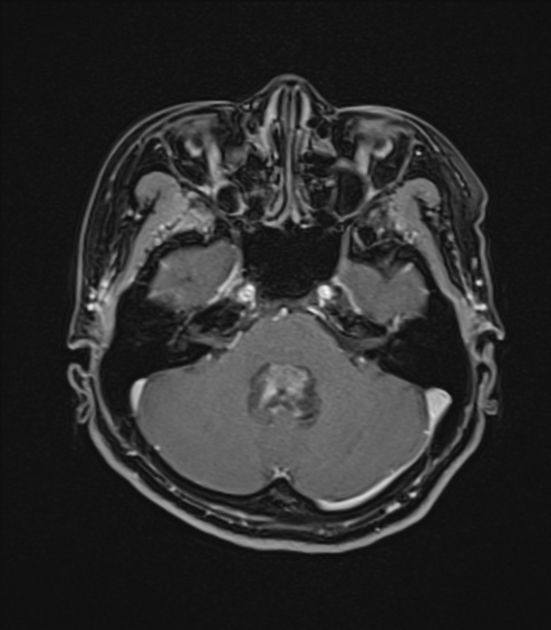
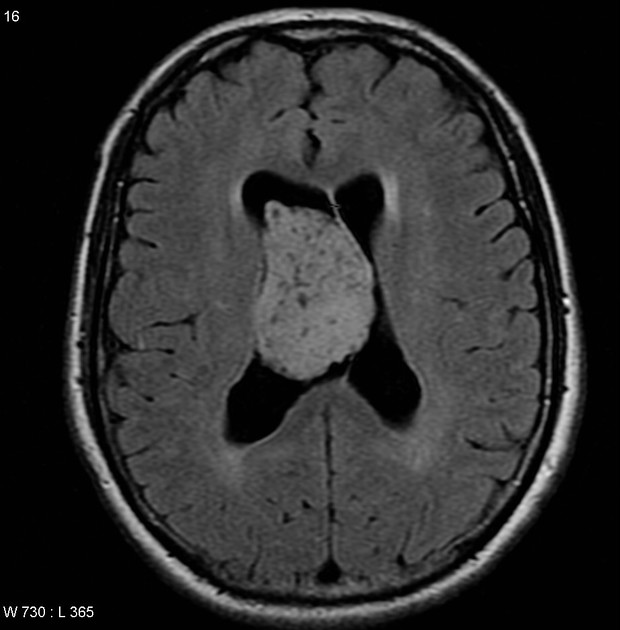
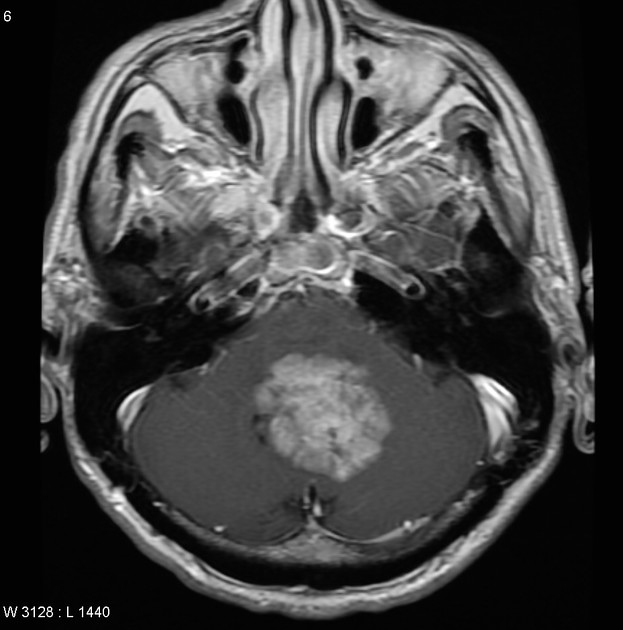
On imaging, these tumours are usually identified in the fourth ventricle in adults and in the lateral ventricles in the paediatric population. They commonly present as a solid vascular tumour with a vivid frond-like enhancement pattern. In a quarter of cases, speckled calcifications are present.
On this page:
Epidemiology
Overall, these tumours account for approximately 1% of all brain tumours, 2-6% of paediatric brain tumours and 0.5% of adult brain tumours. They are, however, disproportionately represented in brain tumours in children under the age of 1 10. Approximately 85% of all choroid plexus papillomas occur in children under the age of 5 years 4.
Interestingly, the age distribution is very different for infratentorial (fourth ventricle) and supratentorial (usually lateral ventricle) tumours. The vast majority of supratentorial tumours are seen in children, whereas posterior fossa tumours are evenly distributed among all age groups, including the elderly 9.
Associations
haemangioblastoma - most frequent
Clinical presentation
Hydrocephalus is very common, seen in over 80% of cases 4. Although the exact mechanism remains uncertain, it is believed to be due to a combination of CSF overproduction and decreased arachnoid granulation resorption.
Pathology
Choroid plexus papillomas are WHO grade I lesions. Their low mitotic rate (<2 mitoses are present per 10 high-power field) and, to a lesser degree, histological features distinguish them from atypical choroid plexus papillomas (WHO grade 2) and choroid plexus carcinomas (WHO Grade 3) 7,10.
Location
Unlike most other brain tumours, which are more common in the posterior fossa in children and supratentorial compartment in adults, the relationship is reversed for choroid plexus papillomas:
adults: most often (70%) occur in the fourth ventricle
children: most often occur in the lateral ventricles, with a predilection for the trigone
Third ventricular, cerebellopontine angle, parenchymal, and even pineal region tumours have also been described.
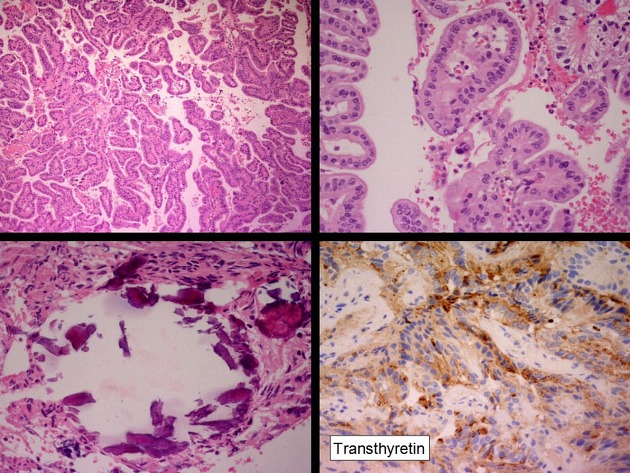
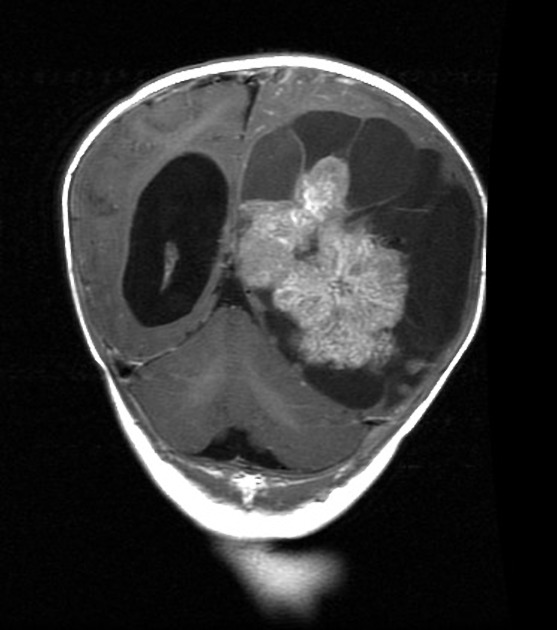
Macroscopic appearance
Choroid plexus papillomas typically appear as cauliflower-like masses 4,10.
Microscopic appearance
These tumours demonstrate papillary structures with a delicate fibrovascular core lined by columnar or cuboidal epithelial cells with vesicular basal nuclei. Their appearance is very similar to normal choroid plexus 7.
Immunophenotype
cytokeratins: positive (especially CK7)
vimentin: positive
-
usually positive
also found in normal choroid plexus
better prognosis if positive 10
-
variable
better prognosis if positive 10
-
usually positive and specific
potassium channel also found in normal choroid plexus 10
Radiographic features
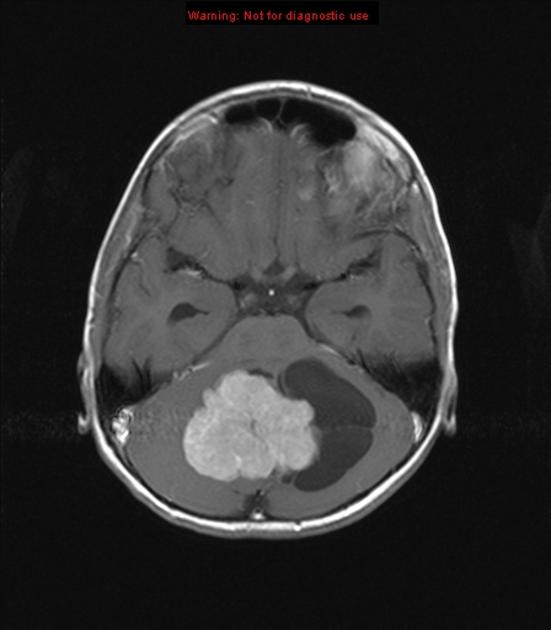
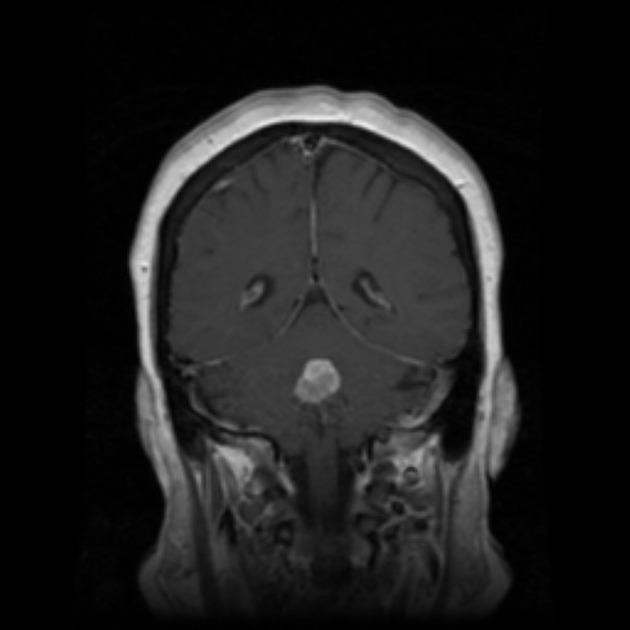
On imaging, choroid plexus papillomas are characterised by vividly enhancing masses, usually intraventricular. Hydrocephalus is common.
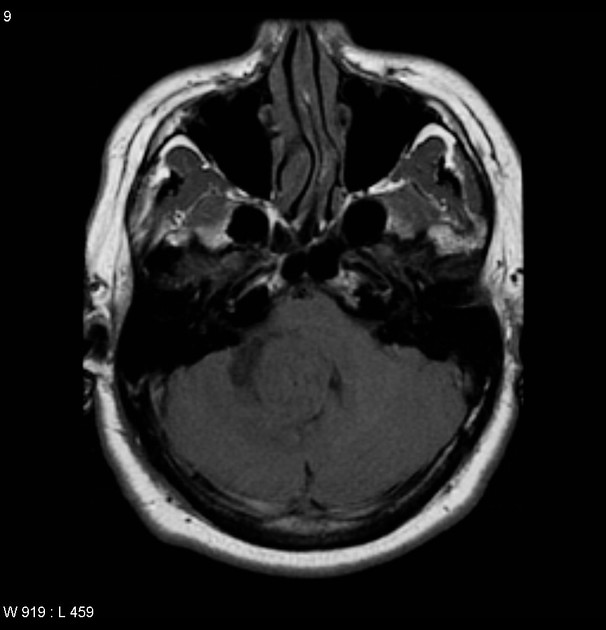
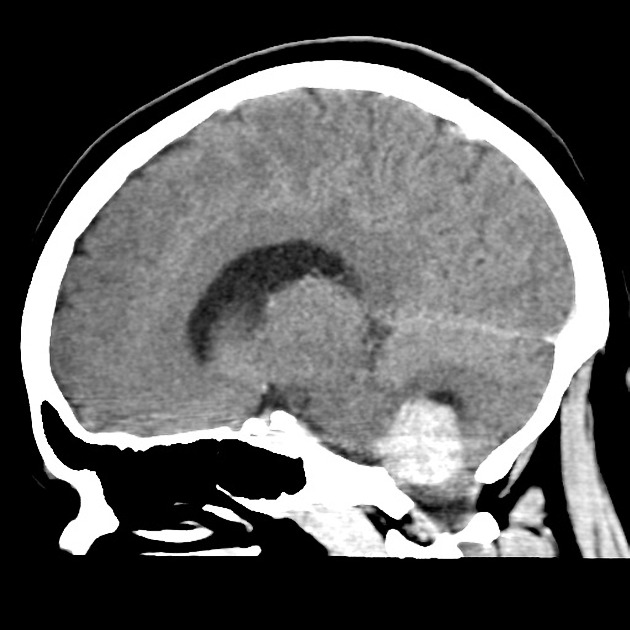
CT
The tumours are usually well-defined lobulated masses, either iso- or somewhat hyperdense compared to the adjacent brain. There is associated hydrocephalus. They usually homogeneously enhance, demonstrating an irregular frond-like pattern, resulting in a cauliflower-like appearance. If there is markedly heterogeneous contrast enhancement, a choroid plexus carcinoma should be suspected 4.
Fine, speckled calcification is seen within the tumour in approximately 25% of cases 4.
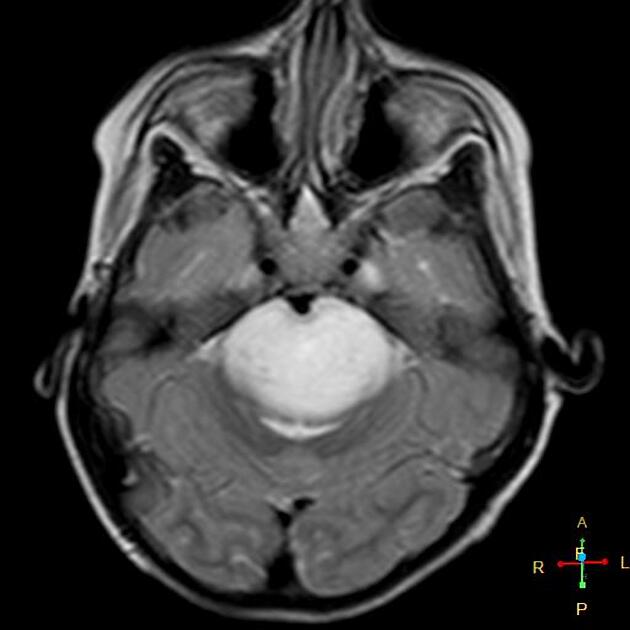
MRI
The frond-like morphology of the tumour can usually be seen, especially following contrast administration. Varying degrees of associated hydrocephalus is also present in almost all cases.
T1: typically isointense compared to the adjacent brain; may be somewhat hypointense
-
T2
iso to hyperintense
small flow voids may be seen within the tumour
T1 C+ (Gd): marked enhancement, tends to be homogeneous
-
MR spectroscopy
decreased NAA
increased Cho
Angiography (DSA)
Being very vascular tumours, these masses demonstrate intense vascular blush on angiography. Enlarged choroidal arteries may be seen feeding the tumour, with shunting 4.
Treatment and prognosis
Total excision should be the aim of therapy and is curative in a vast majority of cases. Overall, there is 90% 1-year-survival, and 77% 5-year-survival 10.
CSF seeding is uncommon in choroid plexus papillomas, but far more frequently seen in higher-grade tumours such as atypical choroid plexus papillomas and choroid plexus carcinomas 10.
Differential diagnosis
The differential is essentially that of other choroid plexus tumours:
atypical choroid plexus papilloma: indistinguishable, but far less common
-
choroid plexus carcinoma: can be very difficult on imaging alone
almost exclusively found in young children 7
heterogeneous contrast enhancement
may show parenchymal invasion
When located in the posterior fossa in children (less common) other tumours to be considered include:
In adults, and depending on location, consider:
exophytic glioma






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.