Ejaculatory duct obstruction refers to the congenital or acquired obstruction of the ejaculatory ducts.
On this page:
Epidemiology
Ejaculatory duct obstruction is rare, accounting for approximately 5% of infertile patients, but thought to be underdiagnosed 2.
Clinical presentation
Patients may present with complaints of oligospermia, aspermia, chronic perineal pain worsened on ejaculation, and rarely infertility 2.
Pathology
Complete or partial obstruction of the ejaculatory ducts may occur as a result of a congenital anomaly such as ejaculatory duct atresia, or be acquired secondary to urogenital infections, urethral trauma or iatrogenic procedures.
Radiographic features
Fluoroscopy
Vasography, which was once the only way to confirm ejaculatory duct obstruction, is no longer performed since newer and less invasive techniques became available such as transrectal ultrasound and MRI.
Ultrasound
Transrectal ultrasound is the modality of choice for the assessment of ejaculatory duct patency 1.
Ejaculatory duct obstruction criteria described on ultrasound are 3
seminal vesicle dilatation: width >15 mm
distension of the ejaculatory duct upstream of the obstacle
stones or calcification within the ejaculatory ducts or the verumontanum
MRI
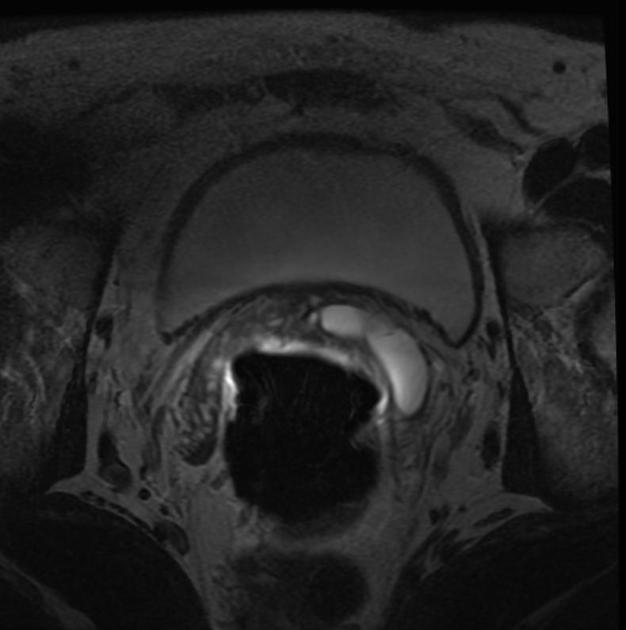
MRI can be performed and demonstrates seminal vesicular dilatation.
Midline cystic lesions of the prostate may be associated.
Treatment and prognosis
Transurethral resection of ejaculatory duct is the standard surgical technique. Newer methods such as recanalization and balloon dilatation following transrectal US-guided seminal vesiculography have also been described 2. In cases where the obstruction is due to calculi, endoscopic laser assisted resection or seminal vesicle lavage are also considered 4.





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.