This is a basic article for medical students and other non-radiologists
Heart failure is a syndrome of cardiac ventricular dysfunction, where the heart is unable to pump sufficiently to meet the body's blood flow requirements.
On this page:
Reference article
This is a summary article; read more in our article on heart failure.
Clinical presentation
Although it is useful to divide the signs and symptoms of heart failure according to the degree of left or right ventricular dysfunction, the heart is an integrated pump, and patients commonly present with both sets of signs and symptoms. Additionally, signs and symptoms may reflect specific causes or aggravators of heart failure.
Left ventricular failure
Patients usually report fatigue, dyspnea on exertion, and if severe, at rest. Orthopnea, paroxysmal nocturnal dyspnea and Cheyne-Stokes respiration can also be a feature.
On examination tachypnea, dyspnea, tachycardia, hypotension and cyanosis may be observed. Palpation may reveal a laterally displaced apex beat while cardiac auscultation may elicit murmurs such as aortic stenosis or mitral regurgitation. Features of pulmonary edema such as inspiratory bibasal crackles not cleared on coughing, diminished breath sounds and dullness to percussion may also be noted.
Right ventricular failure
Symptoms include ankle swelling, fatigue, abdominal bloating/discomfort and nocturia.
Evidence of right ventricular failure can manifest as peripheral edema (if severe extending to thighs and sacrum), ascites, hepatomegaly, elevated jugular venous pressure (JVP). JVP can be further accentuated by hepatojugular reflux. Cardiac murmurs may also be heard, commonly tricuspid regurgitation.
Clinical severity varies significantly and usually classified according to the New York Heart Association, which is graded according to how much physical activity is decreased.
Pathology
Myocardial damage due to myocardial infarcts, cardiomyopathy and myocarditis can cause or aggravate heart failure. Additionally, valvular disease such as aortic stenosis or mitral regurgitation may result in heart failure as well. Further causes include conduction defects, cardiac arrhythmia and infiltrative/matrix disorders.
Systemic factors that may contribute or exacerbate heart failure include anemia, hyperthyroidism or hypertension.
Radiographic features
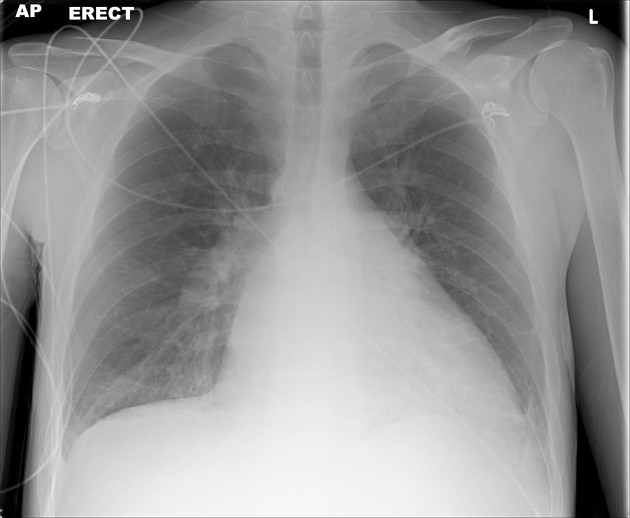
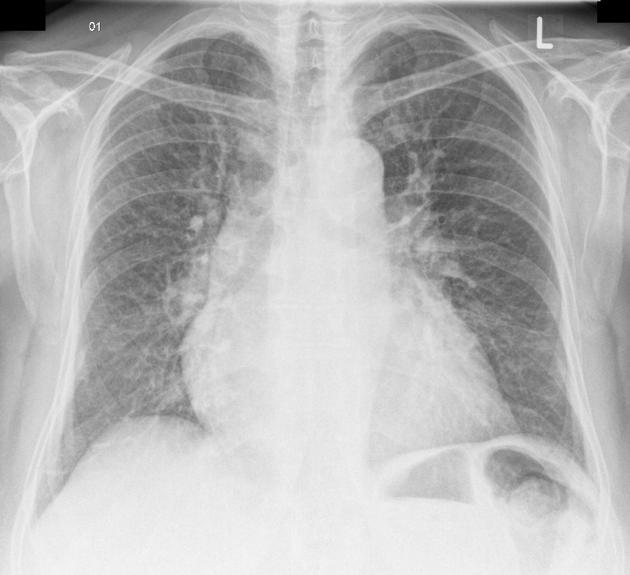
Plain radiograph
Chest x-ray findings include pleural effusions, cardiomegaly (enlargement of the cardiac silhouette), Kerley B lines (horizontal lines in the periphery of the lower posterior lung fields), upper lobe pulmonary venous congestion and interstitial edema.
A good mnemonic to remember these principles is ABCDE:
A - alveolar edema (bat wing opacities)
B - Kerley B lines
C - cardiomegaly
D - dilated upper lobe vessels
E - pleural effusion
Echocardiography
Ultrasound provides an evaluation of the heart chamber dimensions, valvular function, ejection fraction, pericardial effusions and left ventricular hypertrophy.
Treatment and prognosis
Prognosis is usually poor unless the underlying cause is reversed. As a result, patients generally gradually deteriorate with episodes of acute decompensation and ultimately death.
In addition to treating the underlying cause of heart failure, management is directed at dietary and lifestyle changes, medications including ACE inhibitors or beta blockers and if appropriate, implantable cardioverter-defibrillator (ICD) or cardiac resynchronisation therapy (CRT).




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.