Hepatic hemosiderosis
Citation, DOI, disclosures and article data
At the time the article was created Yuranga Weerakkody had no recorded disclosures.
View Yuranga Weerakkody's current disclosuresAt the time the article was last revised Arlene Campos had no financial relationships to ineligible companies to disclose.
View Arlene Campos's current disclosures- Siderosis of the liver
- Hepatic siderosis
- Liver siderosis
- Haemosiderosis of the liver
- Hemosiderosis of the liver
- Liver hemosiderosis
- Hepatic iron overload
Hepatic hemosiderosis, or hepatic iron overload, refers to the deposition of hemosiderin in the liver.
On this page:
Images:
Pathology
Hepatic iron overload can be in the form of 7:
- diffuse
- heterogeneous
- segmental
- focal
- hypersiderosis
- intralesional siderosis
- periportal siderosis
In the absence of genetic hemochromatosis and systemic hemosiderosis, patients with cirrhosis can accumulate focal iron within regenerative or dysplastic hepatic nodules, commonly referred to as 'siderotic nodules'. Siderotic dysplastic nodules are considered premalignant lesions while siderotic regenerative nodules are a marker for severe viral or alcoholic cirrhosis.
Microscopic appearance
Siderotic nodules stain strongly with Prussian blue on histological specimens 6
Radiographic features
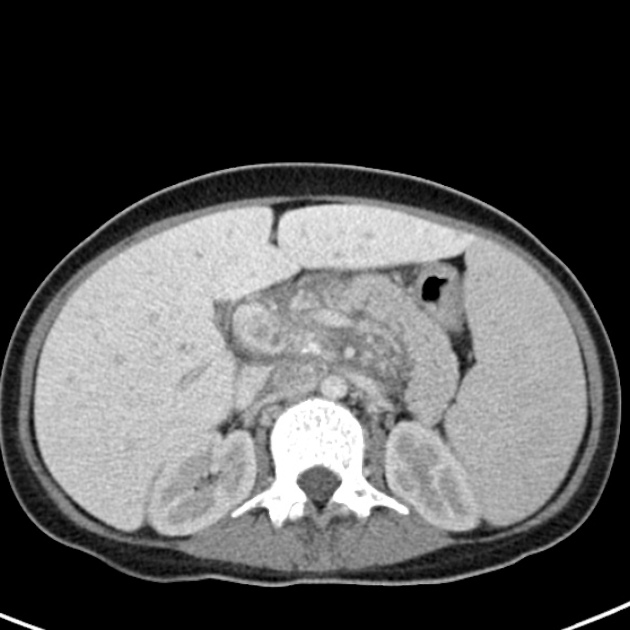
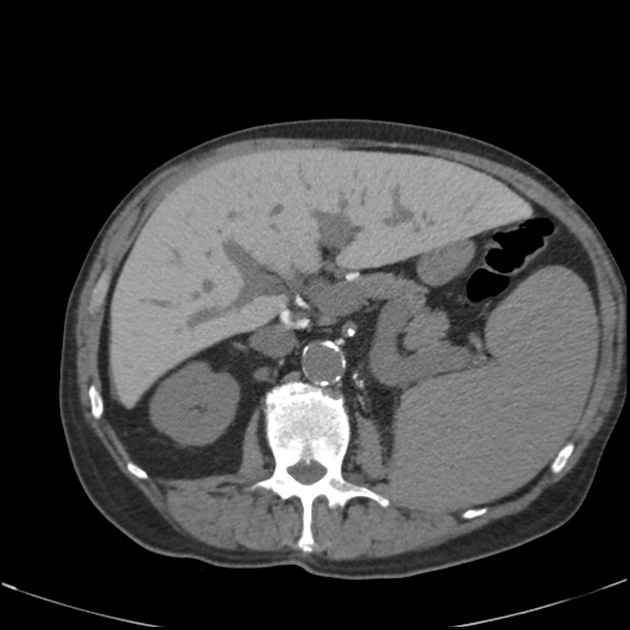
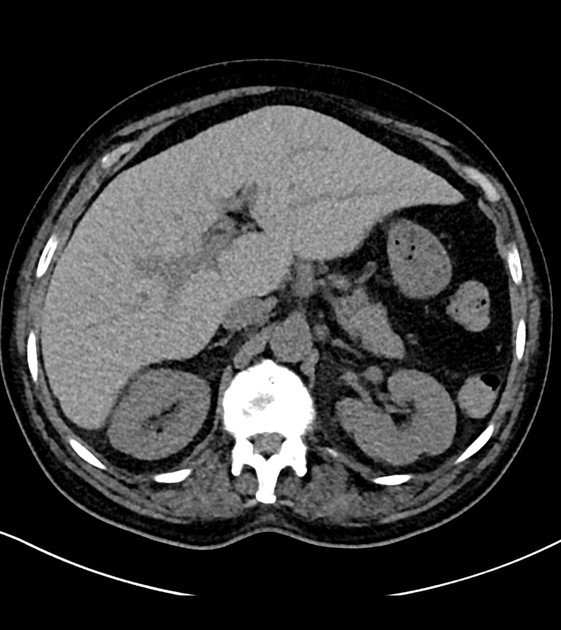
CT
If there are iron deposits above a certain level, siderotic regenerating nodules may appear as high attenuating nodules on CT or as heterogeneous regions of high-density liver parenchyma 3.
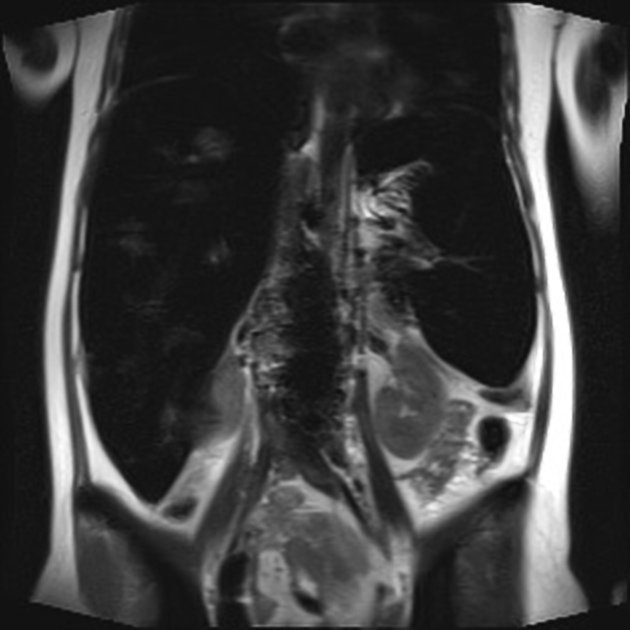
MRI
MRI is more sensitive than CT in demonstrating siderotic regenerating nodules. The detection of siderotic nodules can be improved with the use of GRE pulse sequences with longer TEs 2.
Regenerative siderotic nodules cannot be reliably distinguished from dysplastic siderotic nodules with MR imaging 5.
Reported signal characteristics of hepatic siderotic nodules and diffuse iron overload 2:
- T1: low signal
- T2: low signal
- gradient echo (GRE) with T2* weighting: low signal
- GRE T1-weighted in-phase and out-of-phase sequences: decreased signal on in-phase images compared to out-of-phase images (due to increased T2* effect on the in-phase images, which usually have longer echo times)
MR liver iron quantification is discussed separately.
See also
Quiz questions
References
- 1. Murakami T, Nakamura H, Kuroda C et al. Siderotic Nodules in Hepatic Cirrhosis Disappearing After Biliary Hemorrhage: MR Imaging. J Comput Assist Tomogr. 1991;15(6):1039-41. doi:10.1097/00004728-199111000-00027 - Pubmed
- 2. Krinsky GA, Lee VS, Nguyen MT et-al. Siderotic nodules in the cirrhotic liver at MR imaging with explant correlation: no increased frequency of dysplastic nodules and hepatocellular carcinoma. Radiology. 2001;218 (1): 47-53. Radiology (full text) - Pubmed citation
- 3. Murakami T, Nakamura H, Hori S et-al. CT and MRI of siderotic regenerating nodules in hepatic cirrhosis. J Comput Assist Tomogr. 16 (4): 578-82. - Pubmed citation
- 4. Zhang J, Krinsky GA. Iron-containing nodules of cirrhosis. NMR Biomed. 2004;17 (7): 459-64. doi:10.1002/nbm.926 - Pubmed citation
- 5. Krinsky G, Lee V, Nguyen M et al. Siderotic Nodules at MR Imaging: Regenerative or Dysplastic? J Comput Assist Tomogr. 2000;24(5):773-6. doi:10.1097/00004728-200009000-00019 - Pubmed
- 6. Chandarana H, Lim RP, Jensen JH et-al. Hepatic iron deposition in patients with liver disease: preliminary experience with breath-hold multiecho T2*-weighted sequence. AJR Am J Roentgenol. 2009;193 (5): 1261-7. doi:10.2214/AJR.08.1996 - Pubmed citation
- 7. İdilman İ, Akata D, Özmen M, Karçaaltıncaba M. Different Forms of Iron Accumulation in the Liver on MRI. Diagn Interv Radiol. 2016;22(1):22-8. doi:10.5152/dir.2015.15094 - Pubmed
- 8. Queiroz-Andrade M, Blasbalg R, Ortega CD, Rodstein MA, Baroni RH, Rocha MS, Cerri GG. MR imaging findings of iron overload. (2009) Radiographics : a review publication of the Radiological Society of North America, Inc. 29 (6): 1575-89. doi:10.1148/rg.296095511 - Pubmed
Incoming Links
- β-thalassaemia major
- Sickle cell disease (abdominal manifestations)
- Hyperdense liver due to iron overload
- Sickle cell anaemia: forme fruste
- Macroregenerative siderotic hepatic nodule
- Extramedullary haematopoiesis
- Hepatocellular carcinoma
- Hepatocellular carcinoma containing microscopic (intracytoplasmic) fat
Related articles: Pathology: Hepato-Pancreato-Biliary
- liver
- depositional disorders
- infection and inflammation
- liver abscess
- hepatic hydatid infection
- cirrhosis
- hepatitis
- cholecystitis
- cholangitis
- malignancy
- liver and intrahepatic bile duct tumors
- benign epithelial tumors
- hepatocellular hyperplasia
- hepatocellular adenoma
- hepatic/biliary cysts
- benign nonepithelial tumors
- primary malignant epithelial tumors
- hepatocellular carcinoma
- hepatocellular carcinoma variants
-
cholangiocarcinoma
- intra-hepatic
- mass-forming type
- periductal infiltrating type - Klatskin tumors
- intraductal growing type
- extra-hepatic/large duct type
- intra-hepatic
- biliary cystadenocarcinoma
- combined hepatocellular and cholangiocarcinoma
- hepatoblastoma
- undifferentiated carcinoma
- primary malignant nonepithelial tumors
- hematopoietic and lymphoid tumors
- primary hepatic lymphoma
- hepatic myeloid sarcoma (hepatic chloroma)
- secondary tumors
- miscellaneous
- adrenal rest tumors
- hepatic carcinosarcoma
- hepatic fibroma
- hepatic hemangioma
- hepatic Kaposi sarcoma
- hepatic lipoma
- hepatic mesenchymal hamartoma
- hepatic myxoma
- hepatic rhabdoid tumor
- hepatic solitary fibrous tumor
- hepatic teratoma
- hepatic yolk sac tumor
- inflammatory myofibroblastic tumor (inflammatory pseudotumor)
- nodular regenerative hyperplasia
- pancreatic rest tumors
- primary hepatic carcinoid
- benign epithelial tumors
- liver and intrahepatic bile duct tumors
- metabolic
- trauma
-
vascular and perfusion disorders
- portal vein related
- hepatic artery related
- hepatic veins related
- inferior vena cava related
- other
- third inflow
- liver thrombotic angiitis
- infra diaphragmatic total anomalous pulmonary venous return (TAPVR)
- hereditary hemorrhagic telangiectasia (Osler-Weber-Rendu disease)
- pancreas
-
pancreatic neoplasms
- cystic neoplasm (cystic pancreatic mass differential diagnosis)
- solid neoplasm
- non-epithelial pancreatic neoplasms
- others
- simple pancreatic cyst
-
pancreatitis (mnemonic for the causes)
- acute pancreatitis
- chronic pancreatitis
- Ascaris-induced pancreatitis
- tropical pancreatitis
- autoimmune pancreatitis
- emphysematous pancreatitis
- hypertriglyceridemia-induced pancreatitis
- hereditary pancreatitis
- pancreatitis associated with cystic fibrosis
- pancreaticopleural fistula
- segmental pancreatitis
- pancreatic atrophy
- pancreatic lipomatosis
- pancreatic trauma
- pancreatic transplant
-
pancreatic neoplasms
- gallbladder and biliary
- congenital malformations and anatomical variants
- gallstones
- gallbladder inflammation
- bile ducts inflammation
- gallbladder wall abnormalities
- other gallbladder abnormalities
- bile duct dilatation (differential)
- bile duct wall thickening (differential)
- bile ducts neoplasms





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.