Internal hernias (alternative plural: herniae) are protrusions of the viscera through the peritoneum or mesentery but remaining within the abdominal cavity.
On this page:
Epidemiology
Internal hernias have a low incidence of <1% and represent a relatively small proportion, up to 5.8%, of presentations with small bowel obstruction 1.
Clinical presentation
The most common presentation is an acute obstruction of small bowel loops that develops through normal or abnormal apertures.
Internal hernias not infrequently self-resolve, making imaging at the time of symptomatology vital.
Pathology
The orifice that the small bowel herniates through is usually a pre-existing anatomic structure, such as foramina, recesses, and fossae (e.g. fossa of Landzert).
Pathologic defects of the mesentery and visceral peritoneum can also be secondary to prior surgery, or from congenital maldevelopment of the mesentery.
Types
left and right paraduodenal hernias (most common; ~55% 1)
Radiographic features
In contemporary practice, virtually all patients undergo CT, which is the gold standard imaging modality for assessment of bowel obstruction and suspected internal hernias. Traditionally barium studies were performed and may still on occasion be used in niche circumstances.
CT
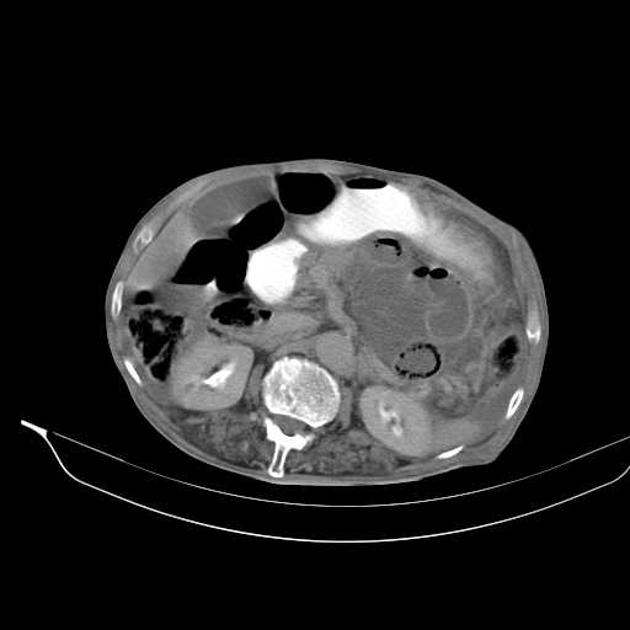
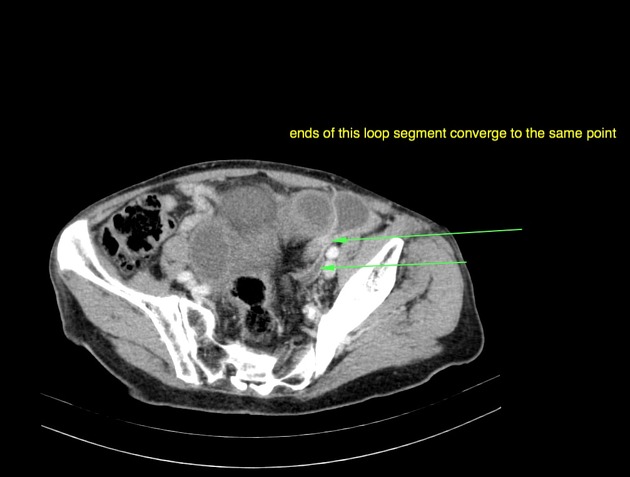
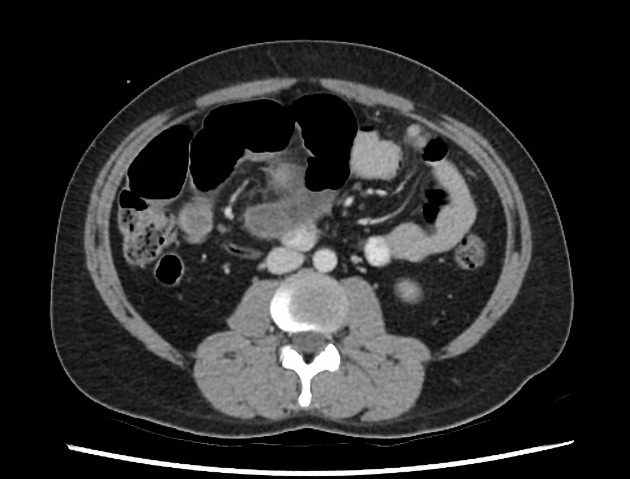
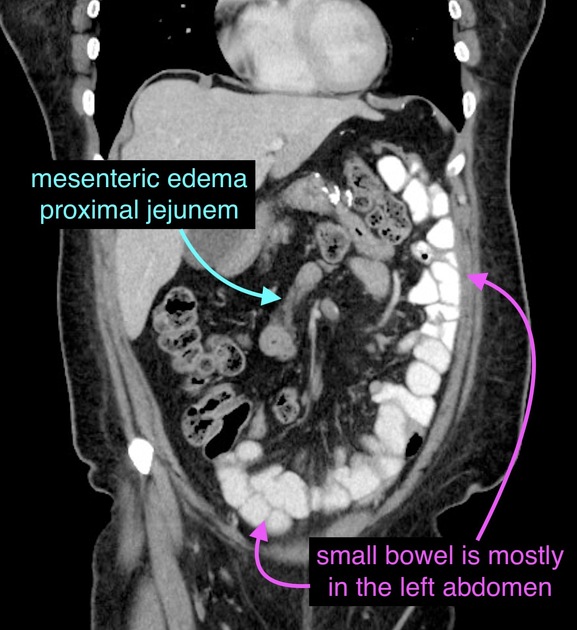
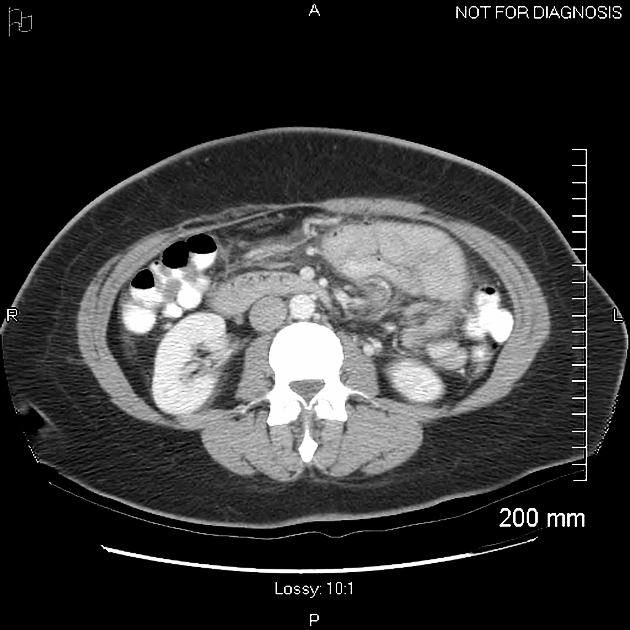
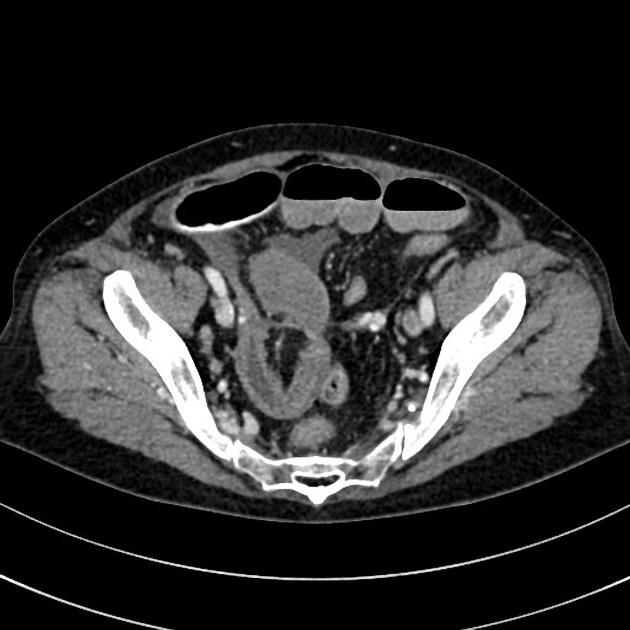
The appearance depends on the particular internal hernia. Common features include:
encapsulation of distended bowel loops within an abnormal location
arrangement or crowding of small bowel loops within a hernial sac
evidence of obstruction with segmental dilatation and stasis
-
mesenteric vessel abnormalities
engorgement, crowding, twisting, stretching of mesenteric vessels
Fluoroscopy
The appearances on barium studies vary depending on the type and site of the internal hernia:
clustering of small bowel loops
distended bowel proximal to the site of obstruction
abnormal site or displacement of normal parts of the gastrointestinal tract
















 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.