Jaundice refers to a clinical sign of hyperbilirubinemia (serum bilirubin >2.5 mg/dL) which has many causes. It is often a clue to a diagnosis. It can be largely divided into two types:
non-obstructive, i.e. prehepatic and hepatic causes
obstructive, i.e. posthepatic causes
Imaging has a major role in detecting the obstructive causes.
On this page:
Clinical presentation
Clinically, jaundice presents with yellowing of the skin, conjunctiva (often incorrectly attributed to the sclerae) 5, and mobile oral tissues (e.g. frenulum, palate) 6. These structures are affected due to their high elastin content, which bilirubin has a high affinity for 6.
It may be painless, painful, or pruritic. Painless jaundice is always very suspicious for an underlying obstructive malignant cause 3.
Pathology
Categories of causes 3:
-
prehepatic
mechanical heart valve
hypersplenism
-
hepatic
-
post-hepatic (or obstructive jaundice)
-
benign causes
strictures, e.g. post-inflammatory/infectious, primary sclerosing cholangitis, traumatic or operative 4
external biliary tree compression, e.g. pancreatic pseudocyst, Mirizzi syndrome
parasites (Ascaris, Clonorchis, Fasciola) 7
-
malignant causes
portal lymphadenopathy
duodenal/ ampullary carcinoma
metastases
-
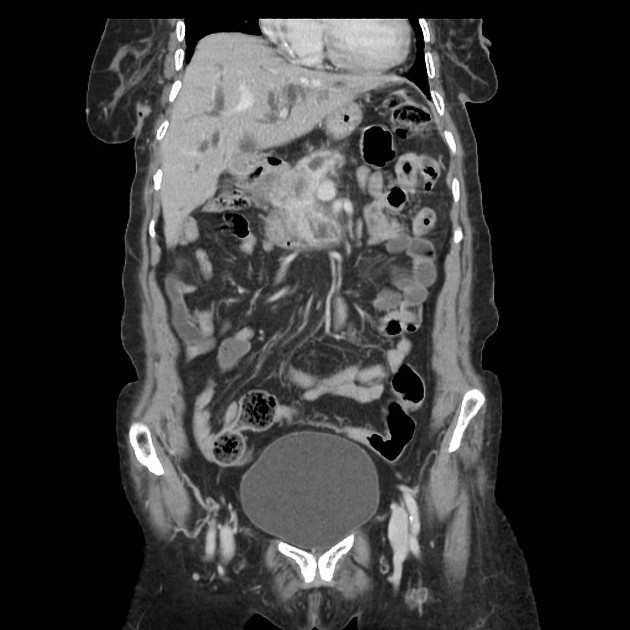
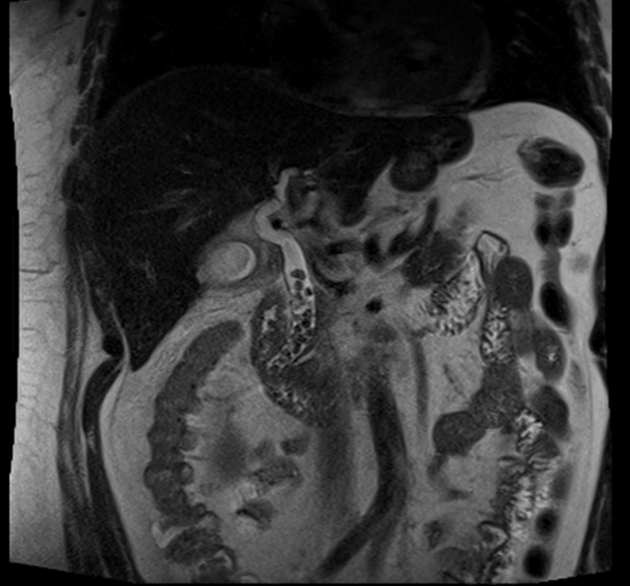
Radiographic features
Jaundice is a common indication for imaging. Often a specific cause will not be found, and the main role is differentiating between a non-obstructive and obstructive jaundice. In the latter, extrahepatic and/or intrahepatic bile duct dilatation can be expected, depending on the level of obstruction.
Hepatobiliary ultrasound and MRCP are the mainstay imaging modalities. Bilirubin levels are often too elevated for CT cholangiography to be performed.
Treatment and prognosis
Management depends on the underlying etiology. In jaundiced neonates, phototherapy and exchange transfusion should be considered.
Complications
bilirubin-induced neurologic dysfunction (e.g. kernicterus) in unconjugated jaundice






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.