Klippel-Trénaunay syndrome is a very rare congenital disorder that is characterised by a triad of venous malformations, cutaneous capillary malformations, and limb overgrowth. It is considered an angio-osteo-hypertrophic syndrome.
On this page:
Terminology
The name Klippel-Trénaunay-Weber syndrome is misleading as the consensus uses two different names to denote two different syndromes. However, they are not always consistently addressed as distinct entities in the literature:
Klippel-Trénaunay syndrome is used in this article, whenever possible
Parkes Weber syndrome with true arteriovenous (AV) shunting
Epidemiology
Most cases of Klippel-Trénaunay syndrome are sporadic and there is no recognised gender or racial predilection. The prevalence of Klippel-Trénaunay syndrome (including Parkes Weber syndrome) is ~1:100,000 11.
Clinical presentation
Klippel-Trénaunay syndrome classically comprises a triad of:
cutaneous capillary malformations: port wine naevi
limb overgrowth: bony or soft tissue hypertrophy of an extremity (localised gigantism)
varicose veins or venous malformations of unusual distribution
The diagnosis of Klippel-Trénaunay syndrome is usually made when any two of the three features are present. Patients usually present in infancy. Features are often unilateral and typically affect one limb 2; capillary malformations may be absent in the atypical form 14. It may be diagnosed in utero 11.
Hypertrophy
Enlargement of the extremity consists of bone elongation, circumferential soft-tissue hypertrophy or both. This often manifests as leg-length discrepancy, although any limb may be affected. Hyperostosis frontalis interna has also been associated with Klippel-Trénaunay syndrome 23.
Capillary malformations
This is the most common cutaneous manifestation of Klippel-Trénaunay syndrome. Typically, capillary malformations involve the enlarged limb, although skin changes may be seen on any part of the body. The lower limb is the affected site in ~95% of patients.
Varicose veins
Present in a majority of patients with Klippel-Trénaunay syndrome, commonly located on the lateral aspect of the affected limb/leg 18 (and in some contradiction to common vena-saphena-magna varicosity). There may be persistence of embryonic veins, of which the lateral marginal vein (the vein of Servelle) has been the most typical finding (68-80% of patients) 22.
Venous malformations can occur in both the superficial and deep venous systems. Superficial venous abnormalities range from ectasia of small veins to persistent embryological veins and large venous malformations. Deep venous abnormalities include aneurysmal dilatation, aplasia, hypoplasia, duplications, and venous incompetence.
Visceral manifestations
Rectal and bladder haemorrhage are serious complications of pelvic vascular malformations and have been reported in 1% of cases 10. Vascular malformations can involve the:
-
gastrointestinal tract (20%)
bleeding is the most common symptom and range from occult bleeding to massive, life-threatening haemorrhages and consumptive coagulopathy
the most frequently reported sites are the distal colon and rectum
upper gastrointestinal bleeding from jejunal haemangiomas may also occur 19
-
genitourinary tract
involved in more severe cases
the absence of severe limb varicosities or venous malformations does not preclude the presence of pelvic involvement
gross haematuria, which is recurrent and painless, is usually the first clinical sign of bladder involvement and frequently manifests early in life
renal hypertrophy and venous enlargement may occur ipsilaterally to the affected side 15
vascular malformations are often located on the anterior bladder wall and dome
the trigone and bladder neck are rarely involved
genital lesions usually do not cause clinical problems for patients with Klippel-Trénaunay syndrome; however, some patients who report erectile dysfunction have abnormal penile veins
-
spleen
splenic haemangiomas may occur 7,20
Skeletal manifestations
These are usually secondary to leg-length difference 13:
ipsilateral hip dislocation
Pathology
Classification
The following levels of severity of Klippel-Trénaunay syndrome have been suggested 13:
venous/phlebectasic dysplasias
arterial dysplasias
-
arterial and associated venous dysplasias
phlebarterectasia (no AV shunt)
angiodysplasias with shunt (i.e. Parkes Weber syndrome)
mixed angiodysplasias: atypical form of Klippel-Trénaunay syndrome
Genetics
Most cases are considered sporadic. However, some of the possible differential diagnoses may have familial predispositions 16.
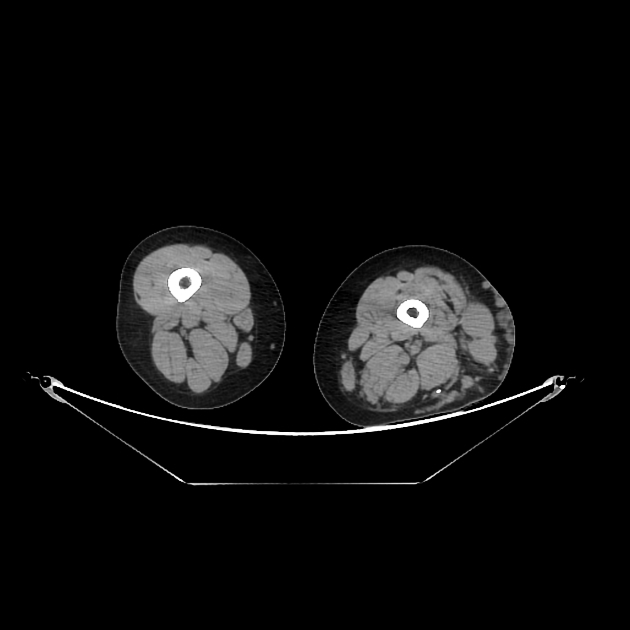
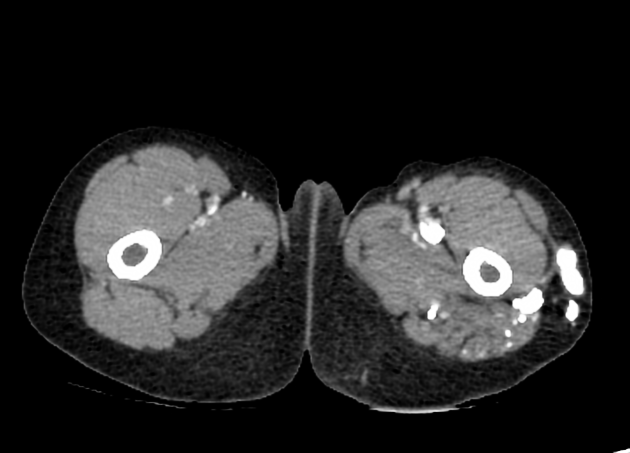
Radiographic features
May show a combination of any of the above mentioned clinical features.
Plain radiograph
On conventional radiography, bone elongation contributing to leg length discrepancy, soft-tissue thickening, or calcified phleboliths may be seen.
Ultrasound
Prenatal ultrasound may diagnose Klippel-Trénaunay syndrome as early as the 15th week of gestation, based on limb hypertrophy and associated subcutaneous cystic lesions. 3D ultrasound may reveal leg width difference. Possible additional features include 11,16:
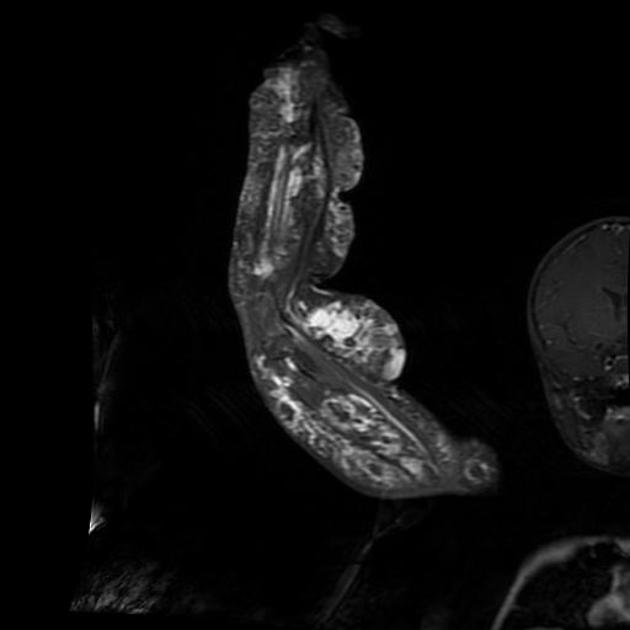
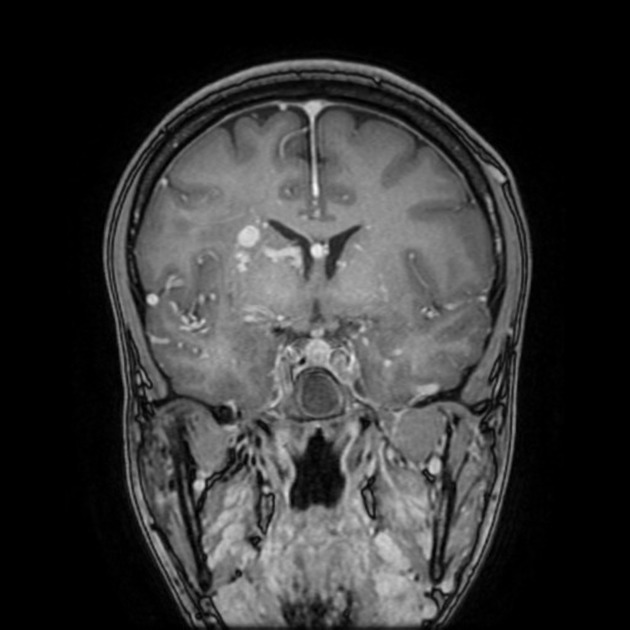
MRI
T2-weighted MR images may show malformed venous and lymphatic lesions as areas of high signal intensity.
MR imaging depicts deep extension of low-flow vascular malformations into muscular compartments and the pelvis and their relationship to adjacent organs as well as bone or soft tissue hypertrophy.
Angiography (DSA)
Typical angiographic findings, which may also be seen on contrast-enhanced CT-scan or MRI, include lower leg superficial varicoid drainage without a deep venous system. The marginal vein of Servelle is a pathognomonic finding (a subcutaneous vein found in the lateral calf and thigh) 9.
Treatment and prognosis
Treatment in a majority of patients is conservative and includes application of graded compressive stockings or pneumatic compression devices to the enlarged extremity. Percutaneous sclerosis of localised venous malformations or superficial venous varicosities may be indicated in some patients. Surgical treatment may include epiphysiodesis to control leg length discrepancy, excision of soft tissue hypertrophy, and stripping of superficial varicose veins.
Complications
thrombophlebitis of the affected limb
venous thromboembolism 21
gastrointestinal or genitourinary haemorrhage if there is visceral involvement (see above)
If capillary malformations are large enough, they may sequester platelets, possibly leading to the Kasabach-Merritt syndrome (consumptive coagulopathy)
History and etymology
In 1900, the French physicians Klippel and Trénaunay first described a syndrome characterised by a capillary naevus of the affected extremity, lateral limb hypertrophy, and varicose veins. In 1918, Parkes Weber noted the association of this triad with arteriovenous fistulas 10-12.
Differential diagnosis
Differentials for intrauterine imaging findings may include 11:
CHILD syndrome (congenital hemidysplasia with ichthyosiform erythroderma and limb defects)
neurofibromatosis type 1 (NF1)
In children and young adults consider:
Parkes Weber syndrome: characterised by AV shunting 24










 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.