Lipomyelocele, also known as lipomyeloschisis, is one of the most common closed spinal dysraphisms. It is most commonly encountered in the thoracolumbar region and usually presents as a fatty subcutaneous mass.
It should not be confused with myeloschisis which is a severe form of open spinal dysraphism.
On this page:
Epidemiology
Lipomyeloschisis, along with the far less common lipomyelomeningocele, account for the majority of all spinal lipomas 3.
Clinical presentation
The diagnosis is usually made clinically due to the presence of a soft, non-tender subcutaneous midline fatty mass just above intergluteal crease 3.
Many (~50%) also have identifiable associated cutaneous abnormalities, including 1-3:
hypertrichosis
atypical dimples
acrochordons (pseudo-tails)
lipomas
haemangiomas
aplasia cutis
dermoid cyst or sinus
Affected individuals are usually neurologically asymptomatic at birth. As the spinal canal grows, there is a distortion of nerve roots with growth thereby leading to neurological deficits, highlighting the importance of early diagnosis and treatment.
Pathology
There is premature separation of surface ectoderm before the formation of proper neural tube with the ingress of mesoderm (which forms fatty elements). The mesoderm prevents proper neurulation.
Radiographic features
MRI
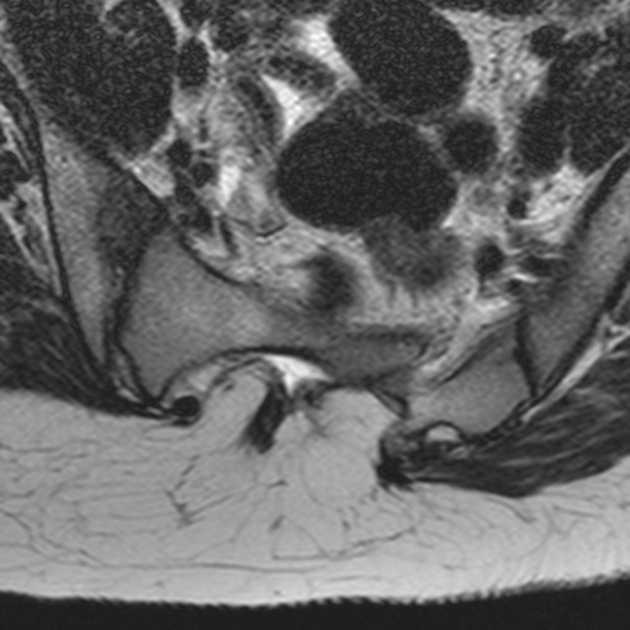
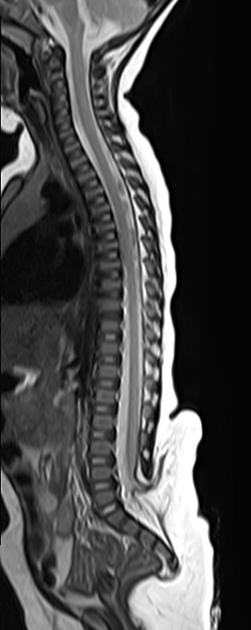
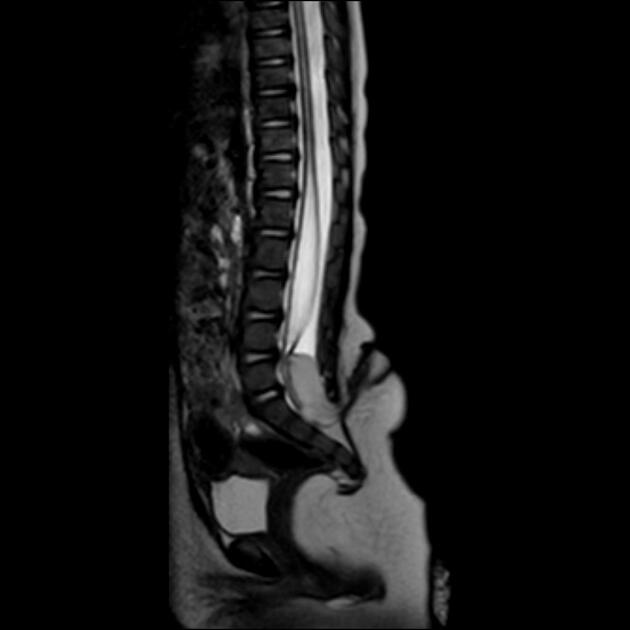
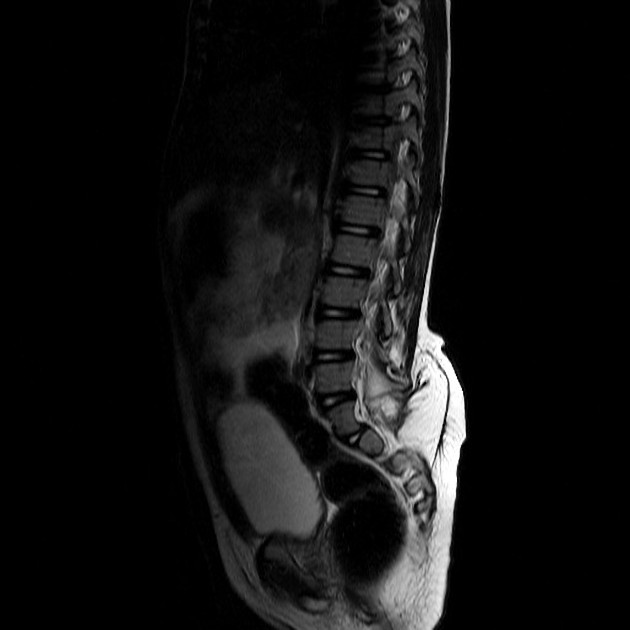
Posterior spinal defect noted which is covered with skin and shows interspersed lipomatous tissue. The neural placode-lipoma interface lies within the spinal canal or at its edge with normal anterior subarachnoid space.
There is usually associated tethered low-lying cord or syrinx of the terminal spinal cord.
Differential diagnosis
Clinical differential diagnosis
Closed spinal dysraphism of thoracolumbar region presenting as subcutaneous mass may be due to:
lipomyelocele
terminal myelocystocele
Imaging differential diagnosis
lipomyelomeningocele: the lipoma-placode interface lies outside the spinal canal with resultant enlargement of anterior subarachnoid space








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.