Hemangiopericytomas of the meninges are rare tumors of the meninges, now considered to be an aggressive form of solitary fibrous tumors of the dura. They often present as large and locally aggressive dural masses, frequently extending through the skull vault. They are difficult to distinguish on imaging from the far more common meningioma. Still, they are treated similarly with surgical resection with or without radiotherapy to reduce the risk of recurrence, which is high.
The remainder of the article presents a historical perspective of this entity. For an updated discussion, please refer to solitary fibrous tumors of the dura.
On this page:
Terminology
Hemangiopericytomas have been enigmatic tumors with a long and checkered history of changing name and classification.
They were previously classified as angioblastic subtype meningiomas, then considered to arise from smooth muscle perivascular pericytes of dural capillaries (pericytes of Zimmerman) 3.
It has since been shown that these lesions arise from fibroblasts and are in the spectrum of the solitary fibrous tumors of the dura 4. This is further supported by the fact that both entities share a similar genetic alteration: genomic inversion of 12q13 locus resulting in the fusion of NAB2 and STAT6 genes, the latter expressed and able to be assessed using immunohistochemistry techniques 6.
This resulted in the term being abandoned throughout the body, but for some time it tenaciously persisted in the CNS classification on account of what was felt to be distinctive imaging features.
In the revised 4th edition (2016) of the WHO classification of CNS tumors, it ceased to be a distinct entity but the term remained in use under the compound diagnosis "solitary fibrous tumor/hemangiopericytoma" 6. In the 5th edition (2021) the term was finally officially retired 7. Solitary fibrous tumors grade 2 or 3 are equivalent to hemangiopericytomas 7.
Epidemiology
Hemangiopericytomas accounted for <1% of all intracranial tumors 1. They were typically encountered in younger adults (30-50 years) with up to 10% being diagnosed in children 3. There is a slight male predilection (M:F = 1.4:1) 3,6.
Clinical presentation
Clinical presentation was usually due to mass effect and will vary depending on location. Headache, seizures, focal neurological dysfunction may all be presenting features 3. Additionally, in up to 20% of cases, these tumors can metastasize systemically, typically to liver, lung, and bone 1,3,6.
Pathology
Solitary fibrous tumors of the dura can be graded from WHO grade 1 to 3 with what traditionally has been termed hemangiopericytomas being grade 2 or 3 6.
Microscopic appearance
Hemangiopericytomas were highly cellular tumors with frequent mitoses (grade II <5 per 10 HPF; grade III ≥5 per 10 HPF) and often with areas of necrosis 6. The cells are separated by a limited amount of delicate reticulin fibers and have numerous "staghorn" vessels, the latter a feature shared by solitary fibrous tumors of the dura 6.
Immunophenotype
Ideally, the diagnosis is confirmed by assessing for STAT6 expression by immunohistochemistry or identifying NAB2-STAT6 fusion 6. Hemangiopericytomas had a number of useful immunohistochemical markers 6:
STAT6: positive
CD34: positive
vimentin: positive
Ki-67 proliferation index is typically around 10% 6.
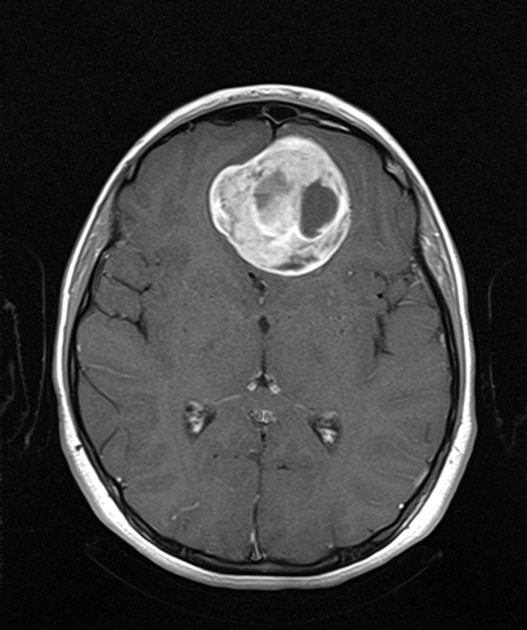
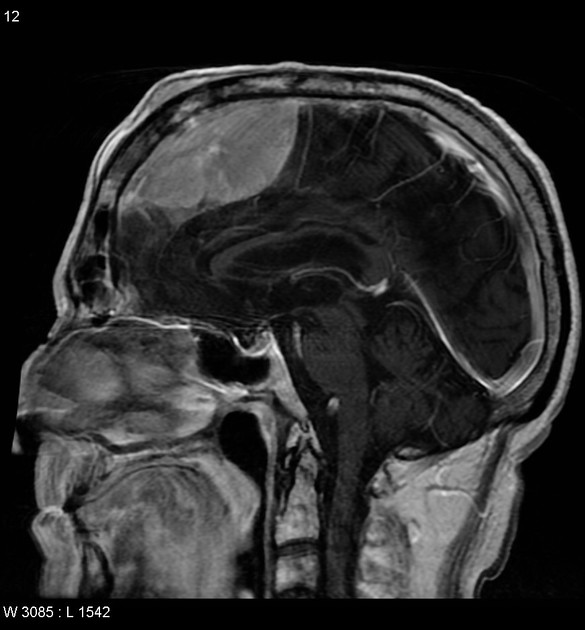
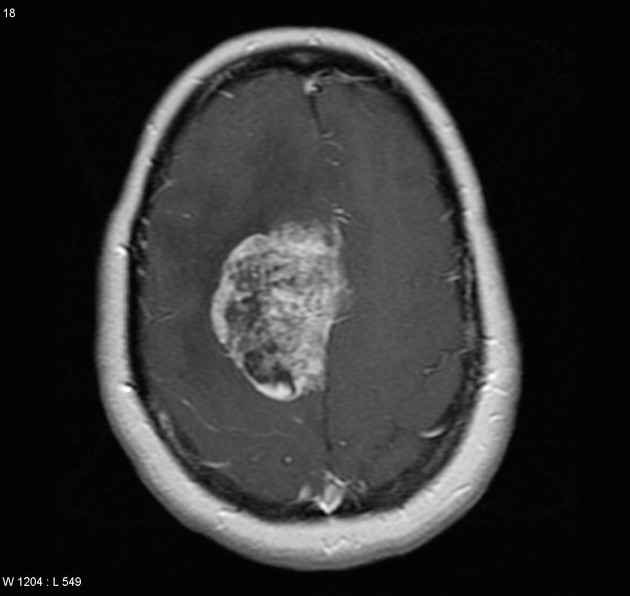
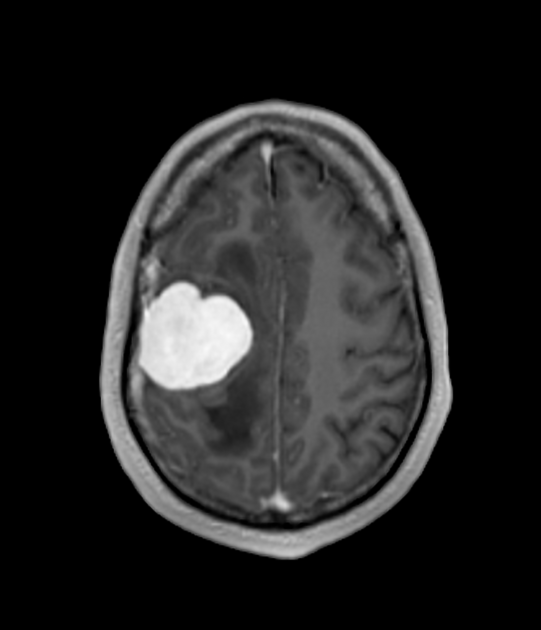
Radiographic features
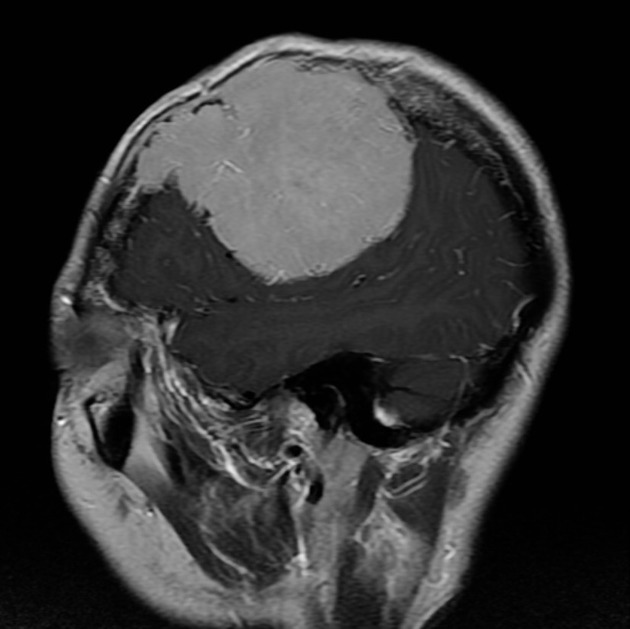
Hemangiopericytomas were almost always solitary, usually supratentorial masses, often lobulated in contour. They were highly vascular and had a tendency to erode adjacent bone 3.
Another common location was the posterior fossa in the posterior occipital region.
CT
vivid enhancement
erosion of adjacent bone
no hyperostosis
no calcification
MRI
Features on various sequences included:
T1: isointense to grey matter
-
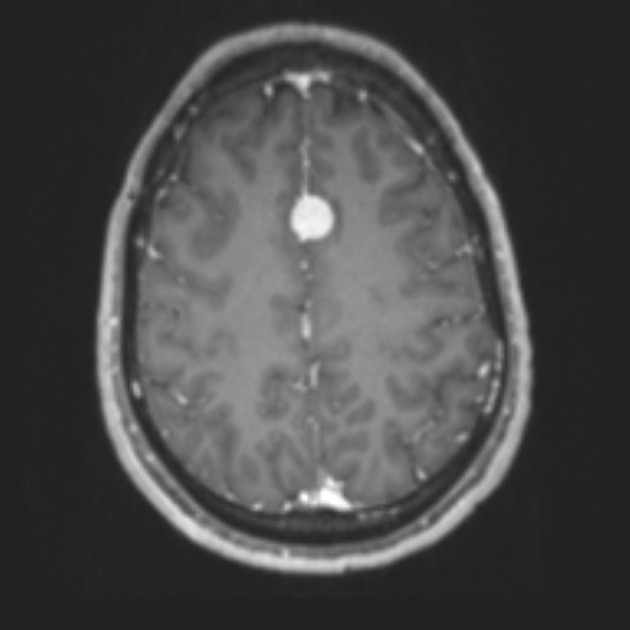
T1 C+ (Gd)
vivid enhancement
heterogeneous
may have a narrow base of dural attachment
dural tail sign is seen, more commonly in grade II tumors
-
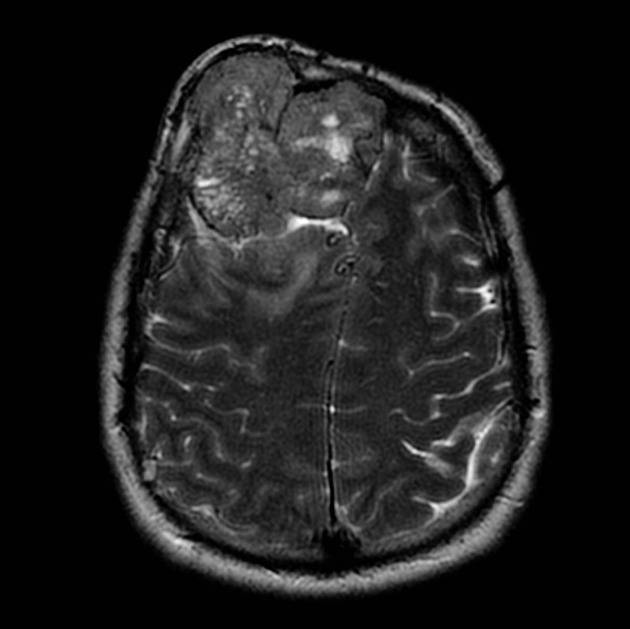
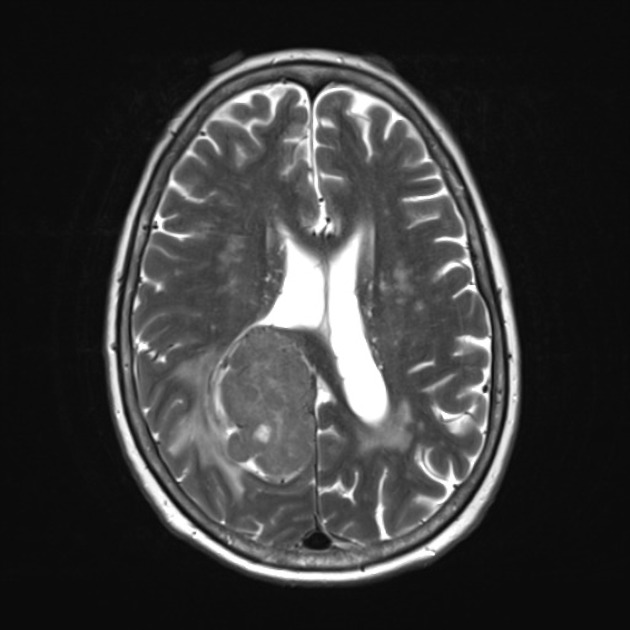
T2
isointense to grey matter
multiple flow voids on MRI (need to distinguish from the spoke-wheel appearance of meningioma)
adjacent brain edema frequently present
-
MR spectroscopy
high myoinositol 3
absent alanine peak (present in meningiomas) 3
-
DWI/ADC
intermediate restricted diffusion (less than meningioma)
minimum ADC ~1100 (+/- 130) x 10-6 mm2/s
Angiography (DSA)
external carotid, internal carotid, and vertebral artery supply common
highly vascular
corkscrew arteries
fluffy tumor stain
lack of early draining veins 3
useful for pre-operative embolization
assessment of dural venous sinus involvement
Treatment and prognosis
Total surgical excision was recommended, with pre-operative catheter embolization helpful in limiting blood loss 3. Adjuvant radiotherapy to reduce the incidence of recurrence has also been advocated 1,3.
Differential diagnosis
The main differential diagnosis was that of meningioma although all other dural masses should be considered. Distinguishing a hemangiopericytoma from a meningioma was difficult as they have similar appearances on both CT and MRI.
-
older patients (>50 years of age)
smoother
central vascular spoke-wheel vascular supply
less likely to erode adjacent bone
more likely to cause hyperostosis
more likely to be multiple
very unlikely to metastasize
usually, have a broad dural attachment and dural tail
MRS: alanine peak, absent myoinositol peak
immunohistochemistry: EMA positive, CD34 and STAT6 negative






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.