A monochorionic diamniotic (MCDA) twin pregnancy is a subtype of monozygotic twin pregnancy. These fetuses share a single chorionic sac but have two amniotic sacs and two yolk sacs.
On this page:
Epidemiology
It accounts for the vast majority (70-75%) of monozygotic twin pregnancies although only ~30% of all twin pregnancies. The estimated incidence is at ~1:400 pregnancies 11.
Pathology
An MCDA pregnancy results from a separation of a single zygote at ~4-8 days (blastocyst) following formation. These fetuses share a single chorionic sac but two yolk sacs and two amniotic sacs. By this time a trophoblast has already formed yielding a single placenta.
The layperson's term is that the twins are "identical". In reality, they are phenotypically similar, and of course of the same gender.
Radiographic features
Ultrasound
First trimester
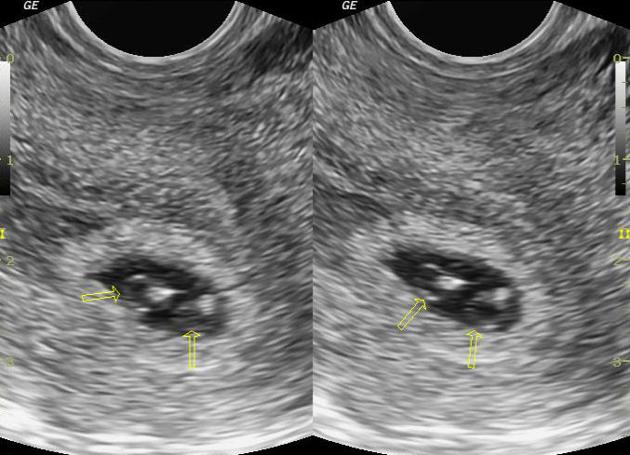
- shows a twin pregnancy with a single gestational sac, and almost always two separate yolk sacs 9,10 (differentiating from an MCMA pregnancy)
- at 14-18 weeks, often a single placenta is seen: differentiating from a DCDA pregnancy
- a thin inter-twin membrane may be seen
- due to amnions abutting the placenta
- present: differentiating from an MCMA pregnancy
- but appears very thin without intervening chorion (often taken as <2 mm): differentiating from a DCDA pregnancy (although this assessment becomes increasingly difficult with the progression of pregnancy)
- T-sign of the intertwin membrane
Second and third trimesters
Findings noted on a second-trimester scan include:
- the number of placental masses, thickness of the membrane, and the presence/absence of the twin-peak sign are still viable options for determining chorionicity
- fetal sex
- almost always the same sex
- in rare circumstances, postzygotic non-disjunction can occur
Negative findings:
- absent twin peak sign: differentiating from a DCDA pregnancy
Treatment and prognosis
Complications
Potential complications that can occur with this type of pregnancy include:
- problems related to abnormal placental vascular anastomoses
- twin to twin transfusion syndrome: can occur in ~15-30% of MCDA pregnancies 1,4
- twin embolization syndrome
- twin reversed arterial perfusion sequence
- demise of one twin: often associated with some adverse outcome to the other twin
- placental insertion related problems
- increased incidence of velamentous cord insertion (cf. singleton pregnancy)
- increased incidence of marginal cord insertion (cf. singleton pregnancy)






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.