Nodular fasciitis (rare plural: nodular fasciitides) is a rapidly spreading non-neoplastic soft tissue lesion that is frequently located in the deep subcutaneous region or in the fascia. The most common locations for nodular fasciitis are the volar aspect of the forearm, the lower extremity, and the chest and back. It typically manifests as a rapidly growing mass.
On this page:
Epidemiology
Most often, nodular fasciitis occurs in patients between 20 and 40 years of age, but children also may be affected.
Clinical presentation
In many cases (~45%), it is localized to the upper extremity, particularly the volar aspect of the forearm. Other common sites are:
trunk (20%)
head and neck (18%)
lower extremities (16%)
Symptoms of tenderness and pain are frequently described at presentation.
Pathology
The pathogenesis of nodular fasciitis is poorly understood. Some describe it as a reactive lesion related to trauma, others have described chromosomal abnormalities that are suggestive of a neoplastic origin.
Location
Three general subtypes of nodular fasciitis may be identified on the basis of the lesion location:
subcutaneous
intramuscular
fascial
Most occurrences of nodular fasciitis are subcutaneous, fascia-based, and circumscribed; these lesions may be amenable to biopsy or excision without any need for imaging evaluation.
Classification
The entity is included in the WHO classification of soft tissue tumors under "fibroblastic/myofibroblastic tumors."
Microscopic appearance
Benign proliferation of fibroblasts and myofibroblasts, typically mistaken for a sarcomatous lesion because of its rapid growth, abundant spindle-shaped cells, and mitotic activity.
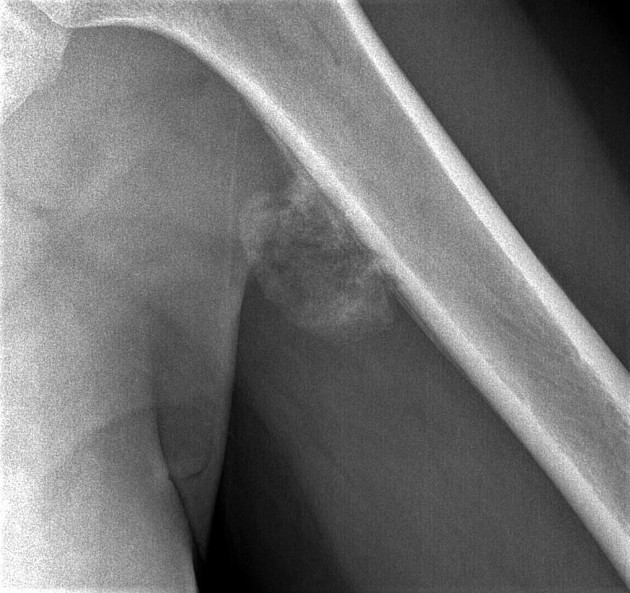
Radiographic features
The lesions tend to be small (<4 cm).
Ultrasound
Sonography can show one or more well-defined isoechoic to hypoechoic nodules with a mildly increased vascular flow in the deep portion of the subcutaneous fat layer, adjacent to or in the fascia.
MRI
Nodular fasciitis may be categorized as myxoid, cellular, or fibrous. This histologic diversity likely accounts for the variable MR imaging appearance of the lesions:
hypercellular lesions appear nearly isointense to that in skeletal muscle on T1WI and hyperintense to that in adipose tissue on T2WI
highly collagenous lesions have hypointense signal on all sequences
contrast enhancement is typically diffuse but may be peripheral
Treatment and prognosis
The imaging-based diagnosis should be confirmed with an excisional biopsy.
Treatment typically consists of marginal excision of the lesion(s). Several weeks of observation (after a diagnosis based on the results of percutaneous fine-needle biopsy) also have been advocated given the self-limited course of the disease. Local recurrence following excision has been reported 6,7.
Spontaneous regression and involution of lesions in response to intralesional steroid injections have been reported 8.
Differential diagnosis
Imaging differential considerations include:
Dupuytren disease (palmar fibromatosis)
extra-abdominal desmoid tumor
if intramuscular early myositis ossificans may be considered
if in the hand, localized tenosynovial giant tumor but this has a peritendinous location and T2* blooming artifact 4









 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.