Olecranon bursitis refers to inflammation of the olecranon bursa. The olecranon bursa is a subcutaneous sac that overlies the olecranon process and contains a small amount of fluid to prevent injury of subcutaneous tissue and skin from the uncovered bony olecranon.
On this page:
Clinical presentation
The presentation is with a tender, fluid-filled olecranon bursa. In cases associated with infection, there may also be overlying inflammatory skin changes (e.g., erythema) and systemic symptoms (e.g., fever) 4.
Pathology
Etiology
Bursitis can develop secondary to many causes:
excessive use - e.g., "student's elbow"
-
trauma
acute trauma
repetitive trauma
infection: septic
inflammation: rheumatoid arthritis, gouty arthropathy, and CPPD
Radiographic features
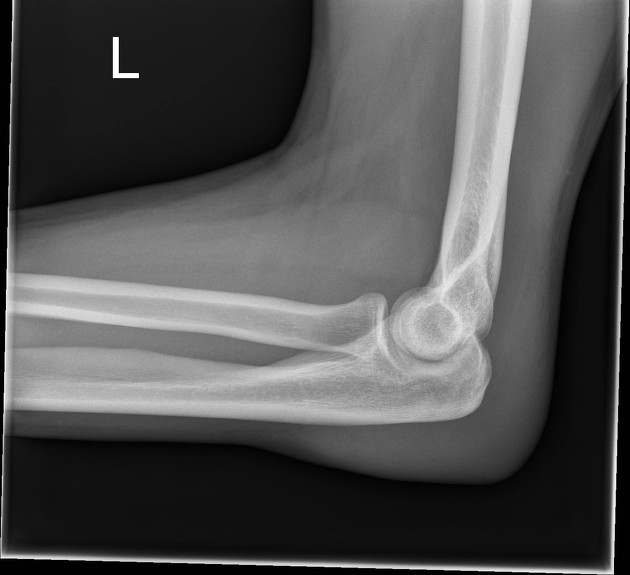
Plain radiograph
Lateral radiographs of the elbow reveal soft tissue swelling superficial to the olecranon 4. An olecranon spur may also be visible 4. A clue to the underlying etiology may also be present, such as traumatic fracture or calcification in gout or CPPD 4.
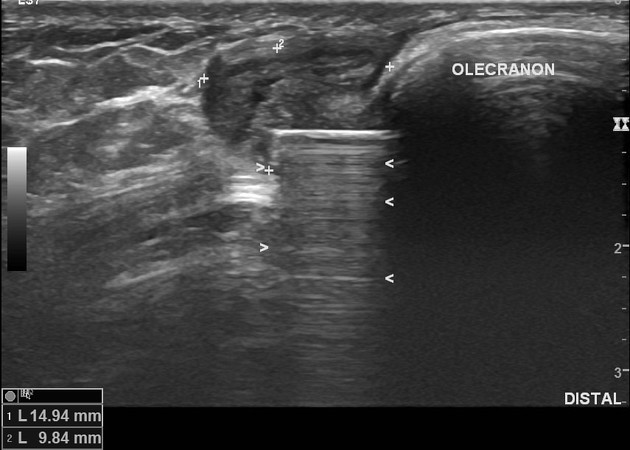
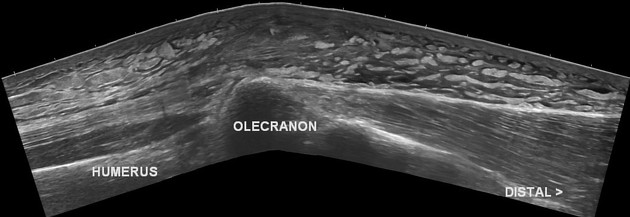
Ultrasound
Ultrasound may show a fluid collection in the olecranon bursa, features of synovial proliferation and/or hyperemia. A small proportion of patients may also show the presence of an associated loose body or features of associated triceps tendinopathy (+/- calcifications) 2.
CT
fluid density at the subcutaneous tissue superficial to the elbow
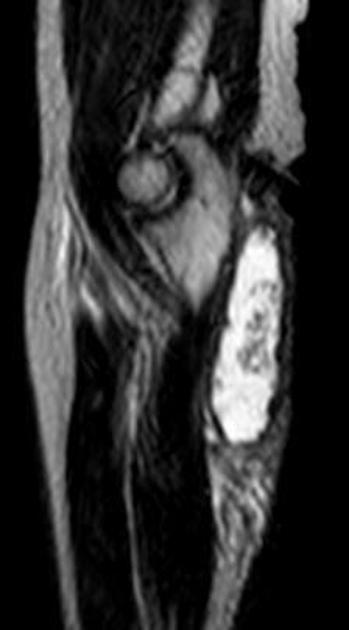
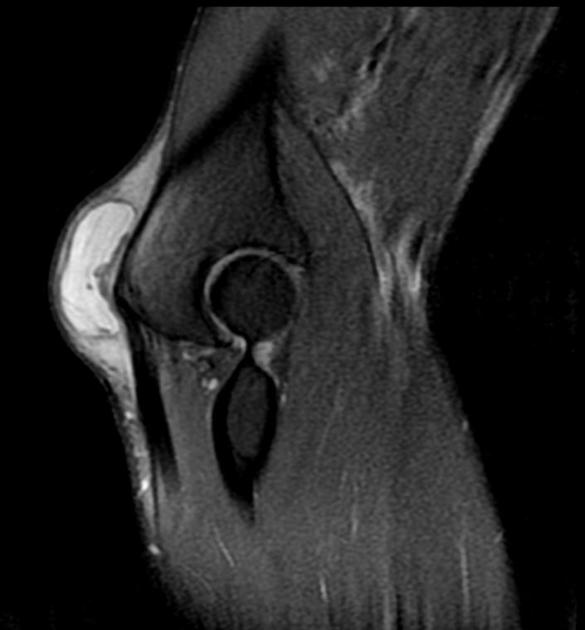
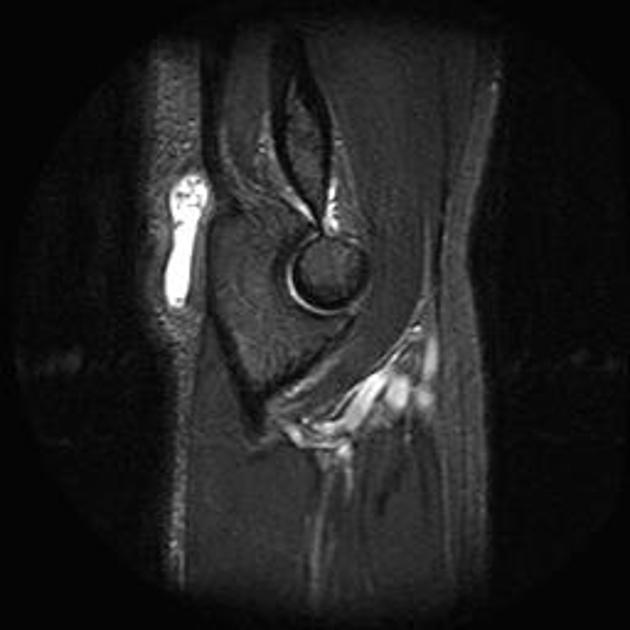
MRI
Bursal fluid collection has the following features:
T1: hypointense
T2: mainly hyperintense
C+ (Gd): enhancement of bursal margins
Triceps brachii muscle and subcutaneous edema as well as elbow joint effusion may be seen.
Treatment and prognosis
Generally, the condition is self-limiting over weeks and there are generally no chronic sequelae if managed conservatively, which includes supportive treatments such as resting, intermittent icing, compression, and simple analgesics (e.g. acetaminophen, NSAIDs) 4,6.
Aspiration of the bursal fluid is generally not required and carries risks (e.g. infection, sinus tract creation), and should be reserved if there is a suspicion of an unusual etiology such as underlying infection 4 or perhaps to relieve significant pressure symptoms 5.
Intrabursal corticosteroid injection is generally not recommended due to relatively high complication rates (e.g. infection, skin atrophy) 4-6.
Surgical bursectomy and/or olceranon spur resection (if present) is a treatment of last resort in cases refractory to the aforementioned treatments 4,5.












 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.