Opioid-associated amnestic syndrome is a form of opioid neurotoxicity characterized by acute memory loss and bilateral hippocampal diffusion restriction and/or T2/FLAIR hyperintensity on MRI.
On this page:
Epidemiology
About 40 cases have been reported in the English literature as of 2020 1.
Fentanyl is the most commonly associated opioid in this syndrome 1. Polysubstance overdose is common, particularly with cocaine 1.
Clinical presentation
The proposed case definition consists of new-onset amnesia (primarily anterograde with a minor retrograde component) that lasts longer than 24 hours and the following supporting factors 1:
confirmed case: positive toxicology for opioid and bilateral hippocampal injury on CT or MRI
probable case: known history of opioid use and bilateral hippocampal injury on CT or MRI
possible case: positive toxicology, history of opioid use, or bilateral hippocampal injury on CT or MRI
Pathophysiology
The underlying pathophysiology is not understood with various possibilities being proposed including 6:
-
vascular
microemboli of drug contaminants
reversible vasospasm
vasculitis
metabolic e.g. neuronal hypermetabolism
Radiographic features
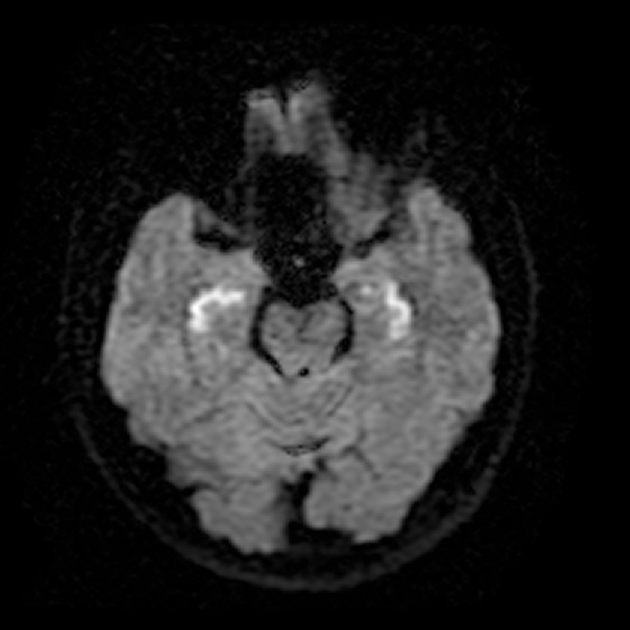
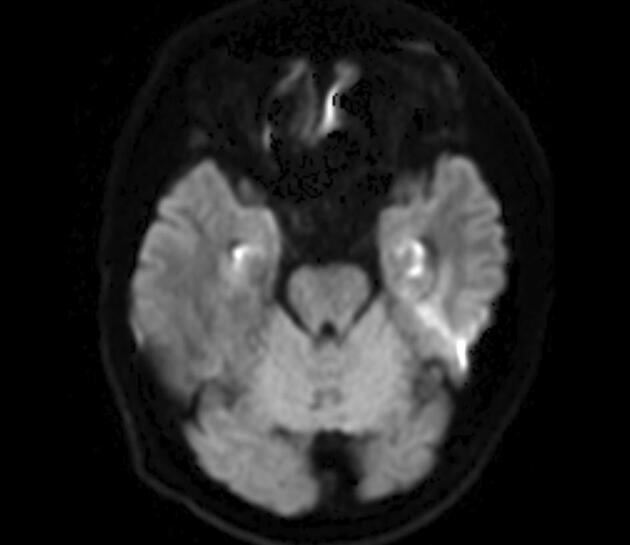
The bilateral hippocampi are symmetrically and diffusely involved 1-4. A wide range of extrahippocampal structures may also be abnormal, including the basal ganglia and cerebellum (cerebellar, hippocampal, and basal nuclei transient edema with restricted diffusion (CHANTER) syndrome).
CT
Non-contrast head CT shows hypodensity of the hippocampi but this finding may be subtle.
MRI
T2/FLAIR: diffuse hyperintensity of the hippocampi is characteristic
DWI: diffusion restriction is a hallmark in the initial days to weeks after injury but resolves thereafter
Treatment and prognosis
No specific treatment has been prescribed, other than cessation of opioid use. General supportive measures and treatment for potential co-morbities (e.g. administering thiamine for potential co-existing Wernicke-Korsakoff syndrome) 6.
Although many patients recover spontaneously within days to week, others have deficits that persist for months or even be permanent 1,6.
Differential diagnosis
In addition to CHANTER syndrome and POUNCE syndrome, that mostly likely exist on spectrum, the imaging differential for causes of bilateral hippocampal restricted diffusion includes hypoxic-ischemic injury (e.g. cardiac arrest), seizures, cardioembolic infarcts, hypoglycemic encephalopathy, and encephalitis 5. Transient global amnesia appears as punctate foci of restricted diffusion, rather than diffuse change.
Clinically, the differential also includes transient global amnesia along with other causes of acute anterograde amnesia such as amnestic syndrome of the subcallosal artery and transient epileptic amnesia.





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.