Osteoarthritis
Updates to Article Attributes
Osteoarthritis (OA), or degenerative joint disease (DJD), is the most common of the arthritides.
Terminology
Because the osteoarthritis is not primarily an inflammatory process, some authors prefer the term osteoarthrosis instead.
Pathology
Primary OA is the less common variant and is characterised by the absence of an antecedent insult, it is considered to be hereditary and affects primarily middle-aged women.
Secondary OA is the most common form, caused by abnormal mechanical forces (e.g. occupational stress and , obesity) or by a previous joint insult (e.g. trauma, rheumatoid arthritis).
Radiographic features
General imaging features
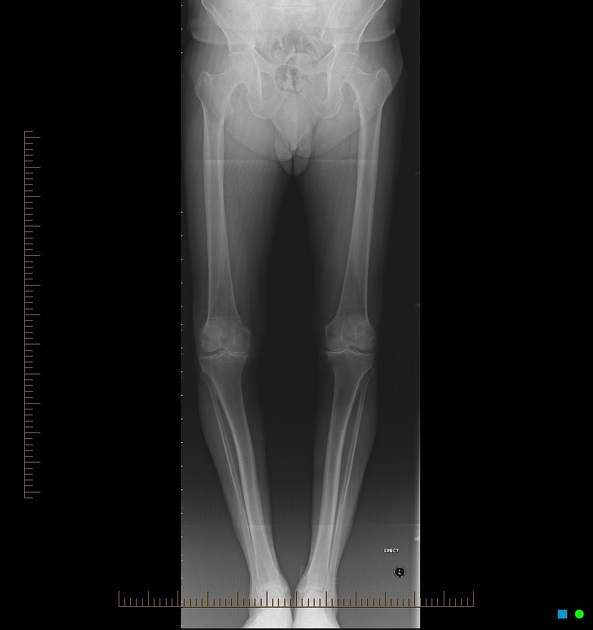
The hallmarks of DJD are joint space narrowing, sclerosis, and osteophytosis. If all three of these findings are not present on a radiograph, another diagnosis should be considered. Joint space narrowing is the least specific finding of the three, yet it is virtually always present in DJD. Unfortunately, it is also seen in almost every other joint abnormality.
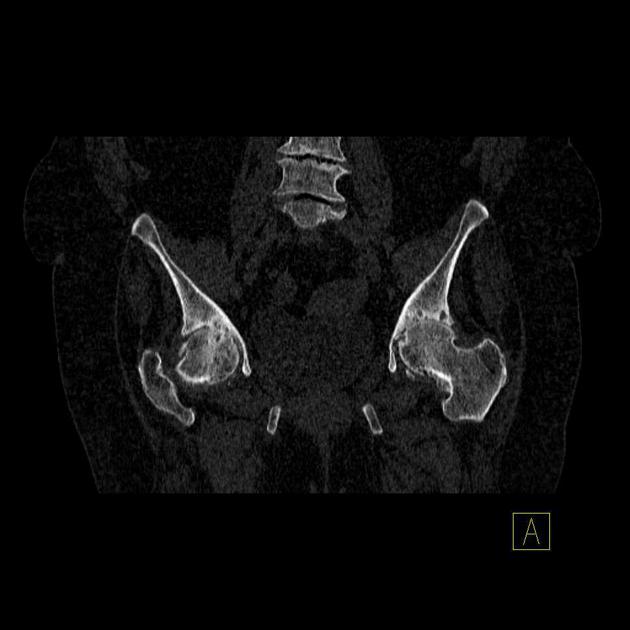
Joint space narrowing: characteristically in osteoarthritis is asymmetric whereas the joint space narrowing in inflammatory conditions is symmetric, e.g. in the hip the narrowing occurs superiorly or sometimes axially in osteoarthritis.
Sclerosis: should be present in varying amounts in all cases of DJD unless severe osteoporosis is present. Osteoporosis will cause sclerosis to be diminished. For instance, in long-standing rheumatoid arthritis in which the cartilage has been destroyed, DJD often occurs with tiny sclerosis.
Osteophytosis: will also be diminished in the setting of osteoporosis. Otherwise, sclerosis and osteophytosis should be prominent in DJD. Some osteophytes carry eponymous names, as discussed bellowbelow.
Primary osteoarthritis is a familial arthritis that affects middle-aged women almost exclusively and is seen only in the hands. It affects the distal interphalangeal joints (Heberden nodes), the proximal interphalangeal joints (Bouchard nodes), and the base of the thumb in a bilaterally symmetric fashion. If it is not bilaterally symmetric, the diagnosis of primary osteoarthritis should be questioned.
There are a few exceptions to the classic triad of findings seen in DJD (sclerosis, joint space narrowing, and osteophytes). Several joints also exhibit erosions as a manifestation of DJD: the temporomandibular joint, the acromioclavicular joint, the sacroiliac joints, and the symphysis pubis. When erosions are seen in one of these joints, DJD must be considered, or inappropriate treatment may be instituted.
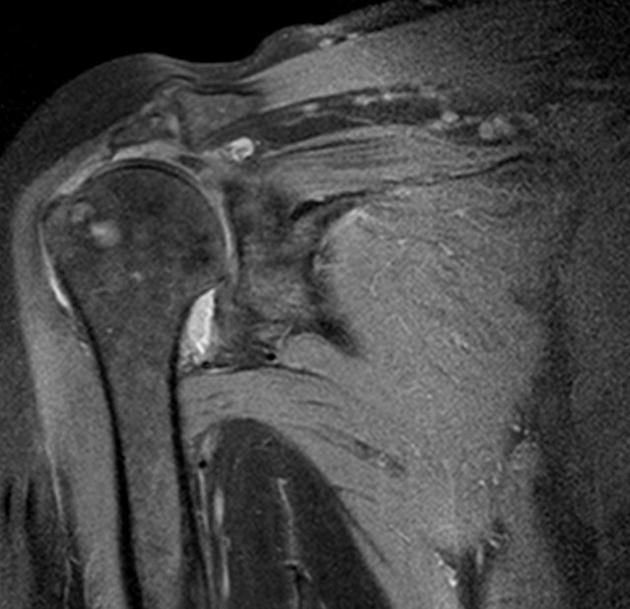
Subchondral cyst or geode: often found in joints affected with DJD. Geodes are cystic formations that occur around joints in a variety of disorders, including: in addition to DJD, rheumatoid arthritis, calcium pyrophosphate dihydrate crystal deposition disease (CPPD) and avascular necrosis. Presumably, one method of geode formation takes place when synovial fluid is forced into the subchondral bone, causing a cystic collection of joint fluid. Another etiology is following a bone contusion, in which the contused bone forms a cyst. They rarely cause problems by themselves but are often misdiagnosed as something more sinister.














 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.