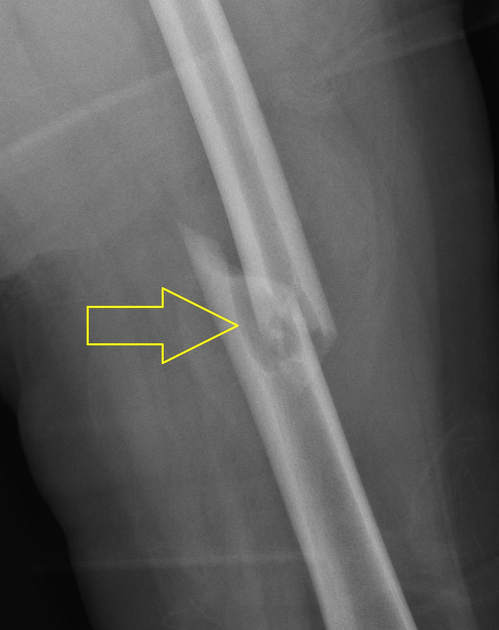
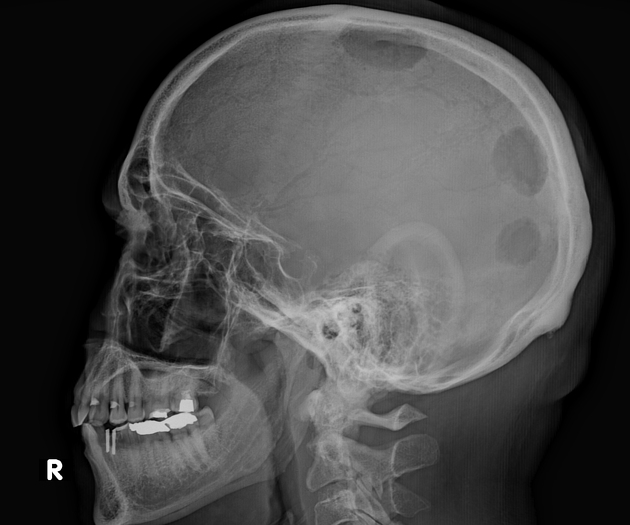
Osteolytic lesions, lytic or lucent bone lesions are descriptive terms for lesions that replace normal bone or with a vast proportion showing a lower density or attenuation than the normal cancellous bone. This comprises lesions with fatty liquid and solid soft tissue components.
On this page:
Pathology
Lucent or osteolytic bone lesions are descriptive radiological terms. Pathologically these findings can be represented by a wide spectrum of conditions including neoplastic, inflammatory and metabolic causes. These lesions are characterised either by the replacement of bone matrix by other types of tissue including soft tissue, fluid or fat. They are the result of uncoupling or imbalance in bone remodelling leading to osteoclast-mediated bone resorption that is triggered by tumour or inflammatory cells and by their surroundings 2,3.
Radiographic features
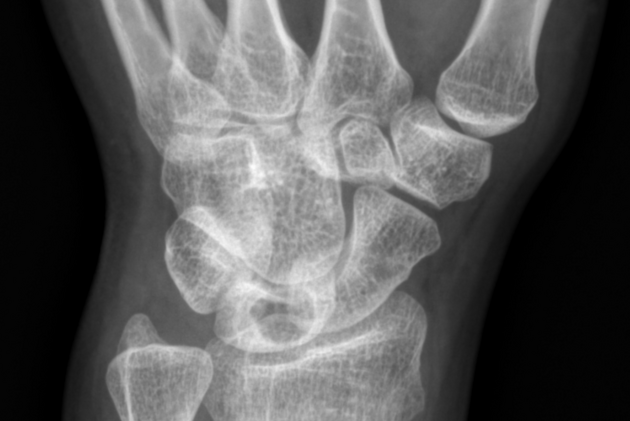
As per definition, osteolytic lesions are radiolucent on plain radiographs and hypodense on CT with lower attenuation than the adjacent trabecular bone 1. This includes lesions with nonsclerotic fatty, liquid or solid soft tissue components. A better and more consistent quantitative definition for the term lucent does not yet exist 1.
Osteolytic lesions can be further characterised by the following 1,4-7:
patterns of bone destruction: geographic, moth-eaten, permeative
margin types: sclerotic, well-defined, poorly defined or indistinct described as wide or narrow zone of transition
cortical involvement: cortical expansion, cortical destruction
periosteal reaction: benign, aggressive
matrix mineralisation: osteoid, chondroid, fibrous
other features: septations and trabeculations
Classification
The radiographic appearance of osteolytic lesions is traditionally classified with the Lodwick classification or the modified Lodwick-Madewell classification. The classification and its modification primarily look at the pattern of bone destruction and the lesion margin including cortical penetration and reflect the aggressiveness of the lesion 4-7.
Differential diagnosis
The differential diagnosis of lucent or osteolytic bone lesions is vast and can be narrowed down according to the following factors 1, 8,9:
aggressive features
history of malignancy
intralesional fatty components
-
location within the bone and the skeleton:
cortical, juxtacortical, centric or eccentric within cancellous bone
axial skeleton, appendicular skeleton, flat bones
typical benign entities
Categorised according to some of the above factors the differential diagnosis includes the following entities 1-3:
presence of aggressive features: see ill-defined osteolytic lesions
absence of aggressive features: see well-defined osteolytic lesions
-
history of malignancy
-
intralesional fatty components
-
typically benign entities
On top of that, age plays an important role in differential diagnosis.
Whereas there is generally a plentitude of possible osteolytic lesions <40 years of age, the most likely differential diagnosis of osteolytic lesions in patients ≥40 years includes the following:
inflammatory conditions: (osteomyelitis, gout)
subchondral cysts/intraosseous ganglion (epiphyses, subarticular regions)
chondrosarcoma (axial skeleton, limb-girdle regions, proximal long bones)
haemangioma (spine)
Practical points
aggressive features: might require an oncological referral and/or biopsy 1
history of malignancy: will almost always require additional imaging, follow-up or oncologic referral
intralesional fatty components in the absence of aggressive features and a history of malignancy: almost always indicate a benign entity













 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.