Passive hepatic congestion, also known as congested liver in cardiac disease or congestive hepatopathy, describes the stasis of blood in the hepatic parenchyma due to impaired hepatic venous drainage, which leads to the dilation of central hepatic veins and hepatomegaly. If there is subsequent hepatic fibrosis, cardiac cirrhosis may develop. Passive hepatic congestion is a well-studied result of acute or chronic right heart failure.
On this page:
Clinical presentation
Symptoms of right heart failure dominate the clinical findings in these patients. Mild right upper quadrant abdominal pain has been reported to be the result of hepatomegaly and stretching of the hepatic Glisson capsule 1. Asymptomatic elevation of serum liver enzymes may also occur 4.
Pathology
Elevated hepatic venous pressure and decreased hepatic venous flow cause hypoxia in hepatic parenchyma and eventual diffuse hepatocyte death and fibrosis. This results in micronodular cirrhosis, indistinguishable from cirrhosis produced by other causes 2.
Aetiology
All forms of heart disease (congenital or acquired) are linked to passive hepatic congestion.
Most common causes of passive hepatic congestion 4-7:
right-sided valvular disease involving the tricuspid or pulmonary valve
pulmonary-related right heart failure, e.g. pulmonary hypertension
congenital heart disease, especially those treated with a Fontan procedure
Radiographic features
Most (80%) patients will have hepatomegaly and severe cases have peripheral oedema, ascites and/or pleural effusions 5.
Ultrasound
Early in the course of the disease, the main abnormality is enlargement of the right hepatic lobe. Normally the right hepatic vein measures <6 mm and, in these patients, its mean is ~9 mm ref.
-
real-time B-Mode
hepatomegaly +/- cirrhosis +/- findings of portal hypertension ref
-
dilated (>2.1 cm) inferior vena cava ref
more specific for elevated filling pressures when lacking respiratory variation (<50%)
elevated filling pressures in the absence of structural cardiac disease may (rarely) imply constrictive pericarditis
-
dilated hepatic veins ref
normal: 5.6 to 6.2 mm
mean diameter: 8.8 mm (in passive congestion)
increases up to 13 mm with pericardial effusion
-
colour Doppler
-
spectral velocity pattern (lVC and hepatic veins)
loss of normal triphasic flow pattern
spectral signal may have an "M" shape
flattening of Doppler waveform in hepatic veins
to-and-fro motion in hepatic veins and IVC
-
-
increased hepatic arterial resistance (RI >0.7)
resistive index (RI) generally between 0.55 and 0.7
this change may be obfuscated by portal hypertension-related shunting, which classically results in a decreased RI
-
pulsatility of the hepatic venous Doppler waveform
prominent a wave and v wave
tricuspid regurgitation may diminish or reverse the S wave
pure right ventricular dysfunction will have a preserved S/D relationship with the amplitude of the S wave > D wave
-
spectral velocity pattern (portal vein)
increased pulsatility of the portal venous Doppler signal
-
cardiac chamber enlargement and/or dysfunction
-
left ventricular systolic or diastolic dysfunction
decreased cardiac index
right and/or left atrial enlargement
valvular stenosis or regurgitation
-
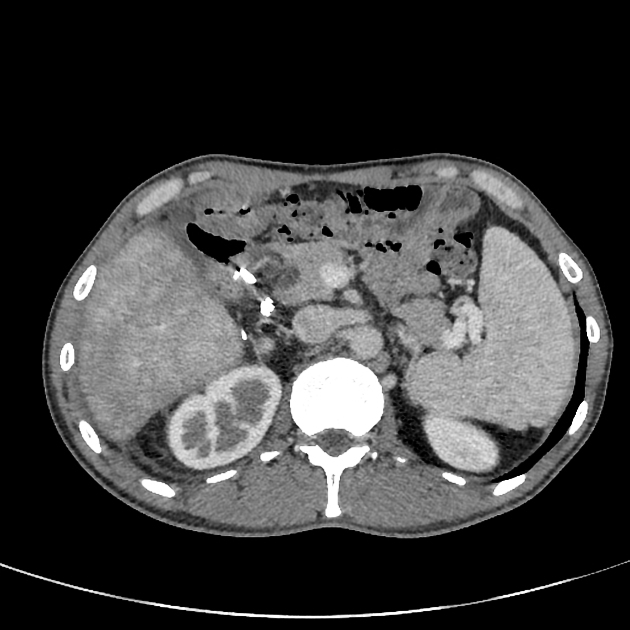
CT
early enhancement of dilated IVC and hepatic veins due to contrast reflux from the right atrium into IVC 9
heterogeneous, mottled and reticulated mosaic parenchymal pattern with areas of poor enhancement, similar to nutmeg liver in Budd-Chiari syndrome 8
peripheral large patchy areas of poor/delayed enhancement
periportal low attenuation (perivascular lymphoedema)
arterial-enhancing (i.e. hypervascular) nodules, which may represent focal nodular hyperplasia (more commonly) or hepatocellular carcinoma (especially in the setting of cirrhosis) 7,8
Chest images may show cardiomegaly and pericardial and pleural effusion 4.
MRI
Macroscopically CT and MRI are able to depict cirrhotic changes as non-specific findings.
-
T1 C+ (Gd)
liver enhancement pattern: reticulated mosaic pattern of low signal intensity linear markings which become more homogenous in 1-2 minutes.
hepatic veins and suprahepatic IVC: early enhancement due to reflux from the atrium
portal vein: diminished, delayed or absent enhancement
fast low-angle shot (FLASH) contrast-enhanced MRI: early reflux of contrast into dilated hepatic veins and IVC
T2: periportal high signal intensity (periportal oedema)
MR angiography: slow or absent antegrade flow within IVC
Differential diagnosis
General imaging differential considerations include ref:
shunting through vascular malformations, e.g. hereditary haemorrhagic telangiectasia







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.