Placenta previa is an abnormally low-lying placenta covering the internal cervical os. As a common cause of antepartum hemorrhage, placenta previa is a potentially life-threatening condition for both mother and infant. As such, antenatal diagnosis is essential to prepare for childbirth adequately.
On this page:
Epidemiology
Placenta previa has an incidence of 1 in 200 pregnancies ref.
Risk factors
Placenta previa is associated with several risk factors, including 8:
previous placenta previa
previous cesarean section
increased maternal age
increased parity
-
large placentas
maternal history of smoking
assisted conception 6
previous manual removal of placenta
Associations
placenta accreta spectrum disorders (~5%): e.g. placenta accreta ref
Clinical presentation
Placenta previa usually presents with painless vaginal bleeding in the second half of pregnancy (>20 weeks gestation), most commonly between 34-38 weeks gestation. Other associated clinical features include:
high fetal presenting part
maternal/fetal compromise secondary to exsanguination
Pathology
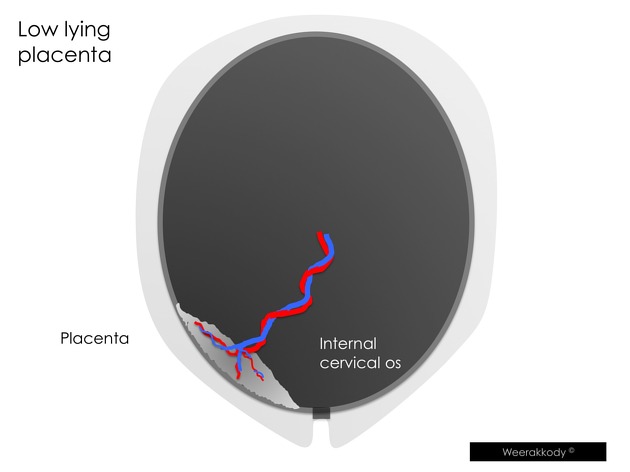
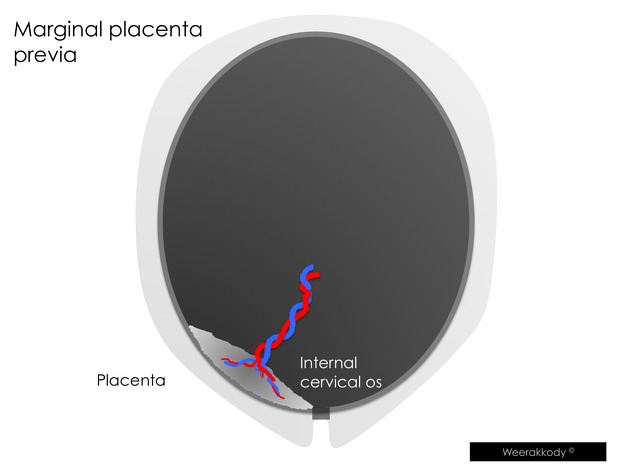
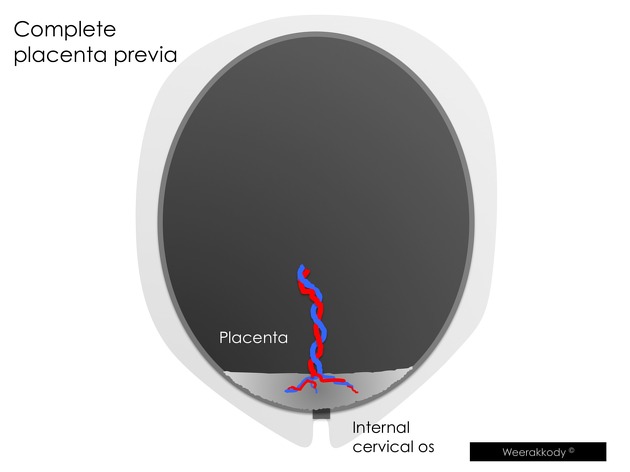
Previously, placenta previa was classified into four grades 5 but due to difficulty in separating grades (i.e. marginal coverage vs partial coverage) the following definitions to describe the relationship of the placental edge with the internal cervical os 8:
placenta previa: placenta covering the internal os
low-lying placenta: placenta <2 cm from the internal os but not covering it
normal: placenta >2 cm from the internal cervical os
Radiographic features
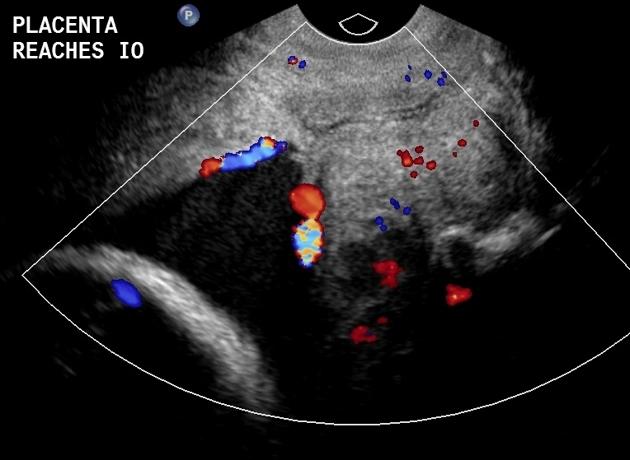
Ultrasound
Due to placental trophotropism, the diagnosis of a placenta previa is not made before 16 weeks 8.
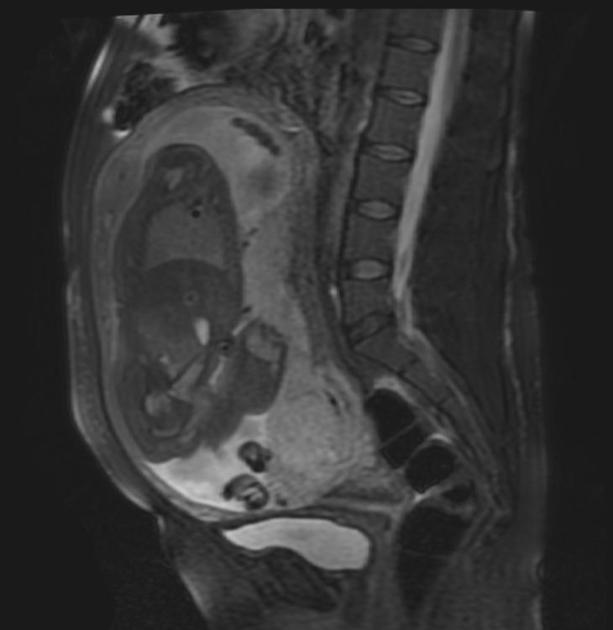
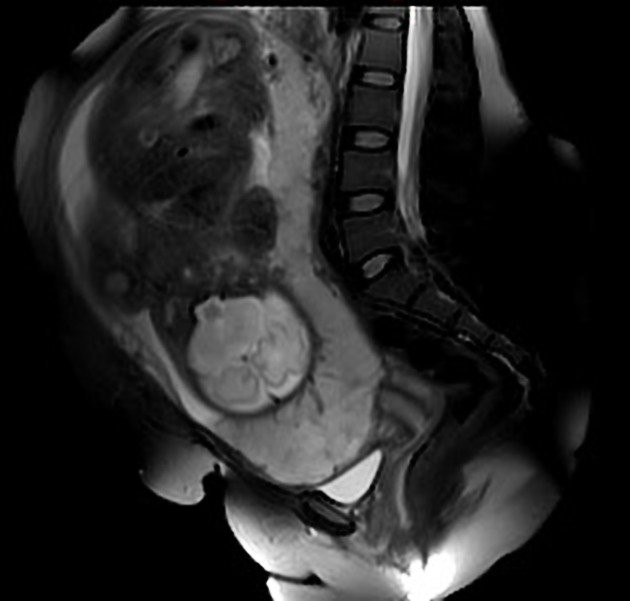
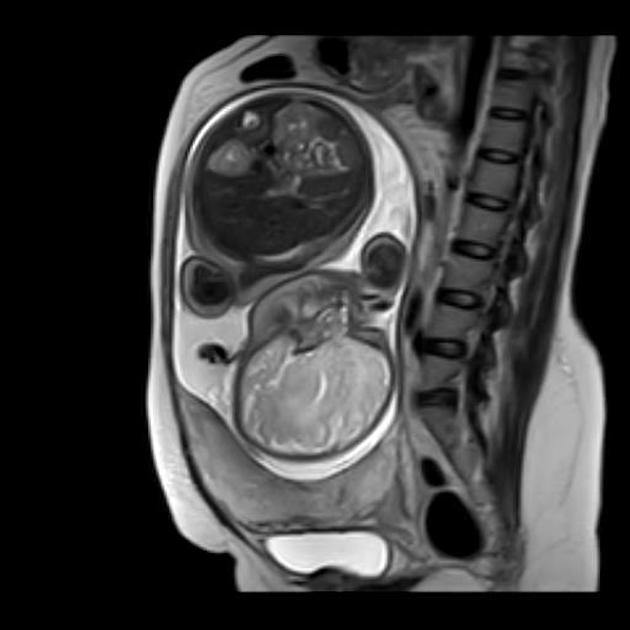
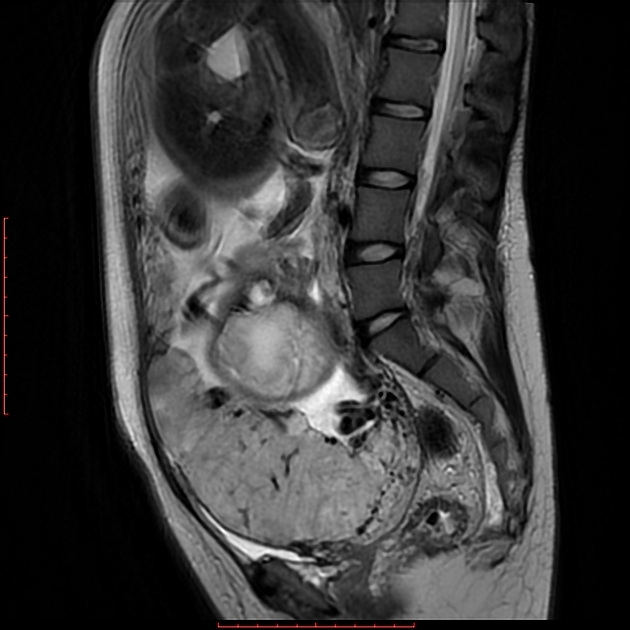
MRI
MRI is the gold standard imaging modality for the placenta and its relationship to the cervix, although in most instances it is not required. Sagittal images best demonstrate the relationship of the placenta to the internal cervical os.
Treatment and prognosis
A low-lying placenta is relatively common in the second-trimester morphology scan, as the fetus grows and the uterus expands, the lower uterine segment thins and grows at a faster rate 8, such that in most cases the placenta is no longer low-lying by a follow-up transabdominal ultrasound. In asymptomatic women, this is recommended at 32 weeks, and if the placenta is persistently low-lying (including placenta previa), a further follow-up transvaginal ultrasound is recommended at 36 weeks 8.
In the case of a complete placenta previa, a cesarian section is required for delivery to avoid the risk of fetal and maternal hemorrhage.
History and etymology
Previa is of Latin origin. It is a combination of 'prae' (meaning before) and 'via' (meaning way).
Differential diagnosis
full bladder
These can make the placenta appear closer to the internal cervical os than it actually is (particularly on a second trimester scan). Postvoid images should always be obtained if previa is suspected.
Occasionally, a subchorionic hematoma that extends over the cervix can mimic placenta previa, especially if the hemorrhage is still echogenic. Follow-up imaging would be useful to distinguish the two entities.
Practical points
transvaginal ultrasound scan is more accurate to assess placenta previa, the transabdominal scan may overdiagnose it in up to one-quarter of cases
when diagnosed in the second trimester, a third-trimester ultrasound scan at 32 weeks should be performed to reassess the placenta position 8





 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.