Plexiform neurofibroma is an uncommon variant of neurofibroma, a benign tumour of peripheral nerves (WHO grade I), arising from a proliferation of all neural elements. Plexiform neurofibromas are essentially pathognomonic of neurofibromatosis type 1 (NF1). Unlike small sporadic localised neurofibromas and diffuse cutaneous neurofibromas (both discussed separately), these tumours are at significant risk of eventual malignant transformation.
On this page:
Terminology
There is variable use and some confusion about the distinction between plexiform neurofibroma and diffuse cutaneous neurofibroma, with some sources not clearly distinguishing between the two. Generally, plexiform neurofibromas are deeper lesions affecting nerves and plexus. The two may, however, co-exist 5.
Importantly it appears that diffuse cutaneous neurofibromas may not be as closely associated with neurofibromatosis type 1 (NF1), nor have the same risk of malignant transformation 1-4. The distinction is thus important.
Epidemiology
Plexiform neurofibromas are usually diagnosed in early childhood. They are found in approximately 30% of patients with NF1.
Clinical presentation
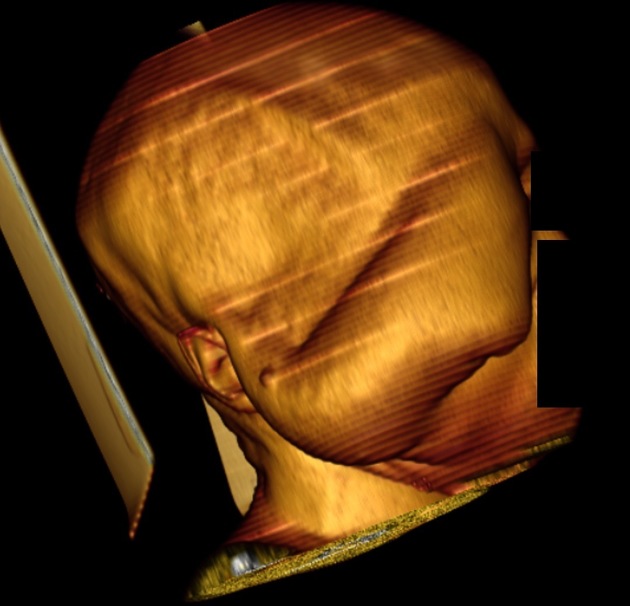
Clinically, it presents as a subcutaneous mass which feels like a "bag of worms". Most of the time, it is a superficial cutaneous/subcutaneous lesion, but it can occur almost anywhere in the body. Symptoms may be related to local mass effect.
Pathology
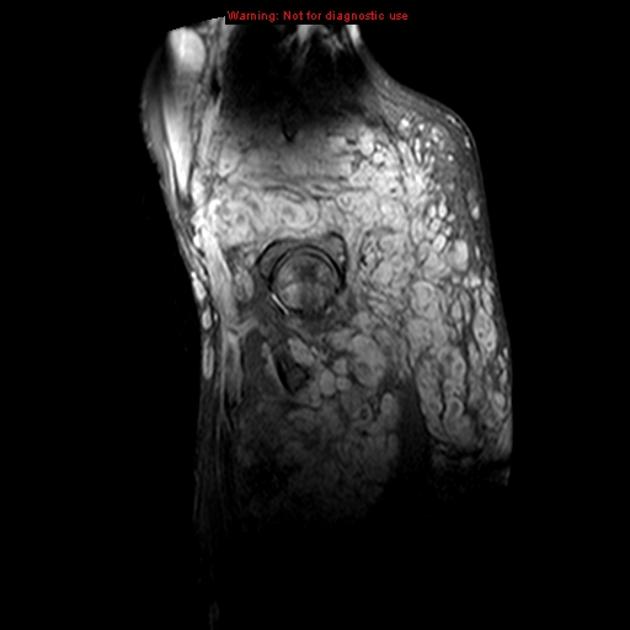
Plexiform neurofibromas diffusely involve long nerve segments and its branches, often extending beyond the epineurium into the surrounding tissue.
Immunophenotype
Immunohistochemistry demonstrates findings in keeping with a neurogenic origin, including 6.
S100: positive (fewer reactive cells than in schwannoma)
SOX10: positive (fewer reactive cells than in schwannoma)
neurofilament: only positive in entrapped axons
Radiographic features
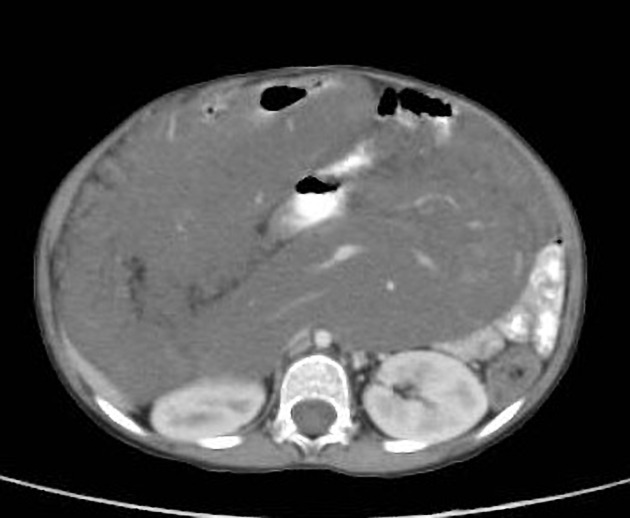
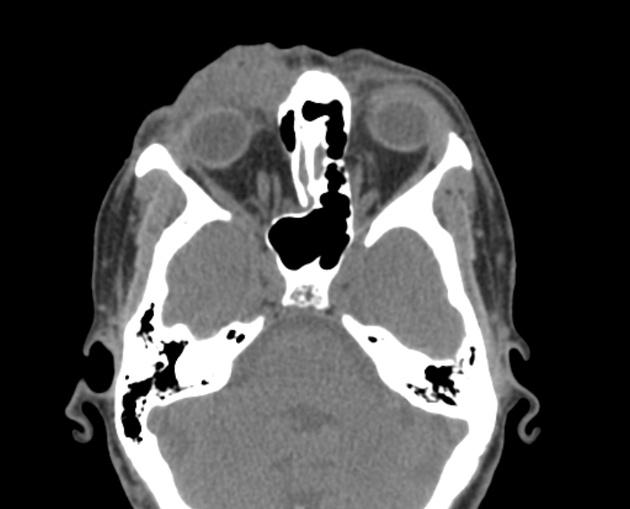
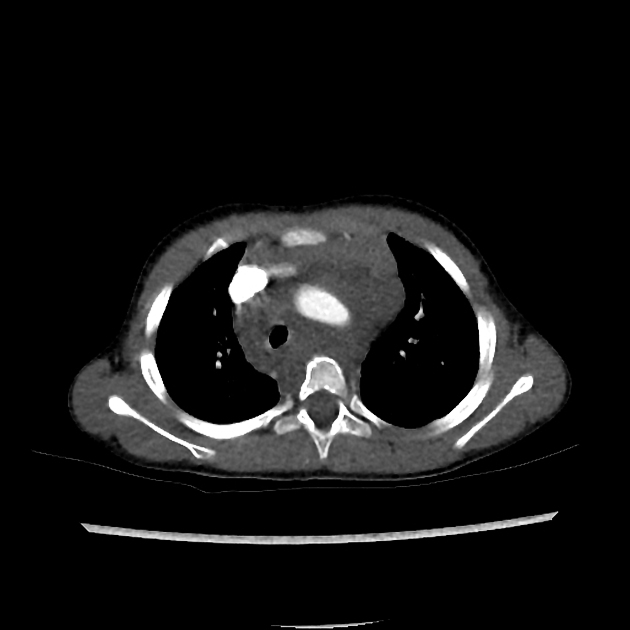
CT
Non-specific infiltrative subcutaneous lesions.
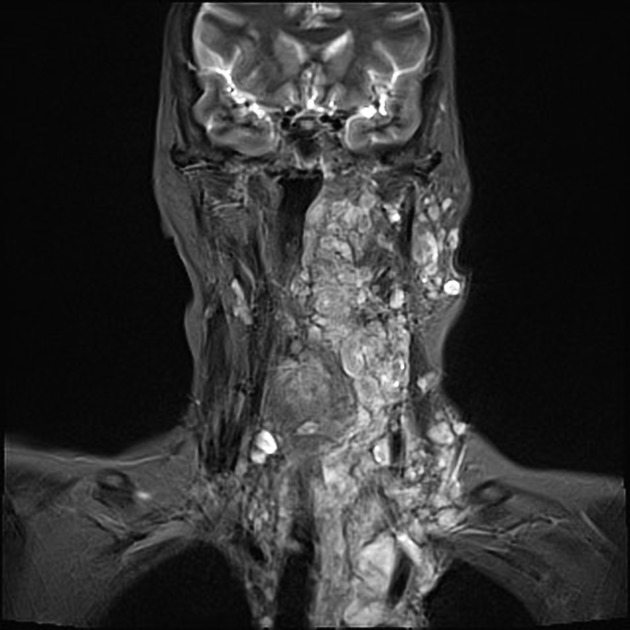
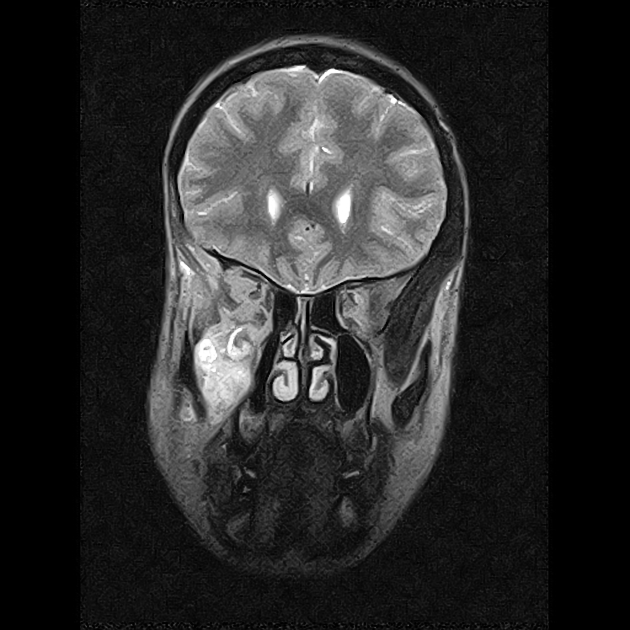
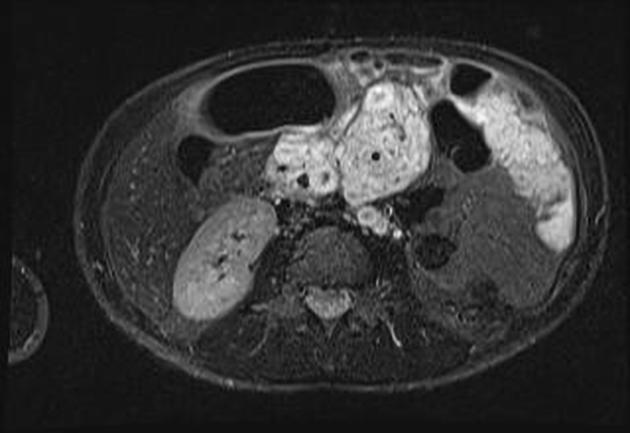
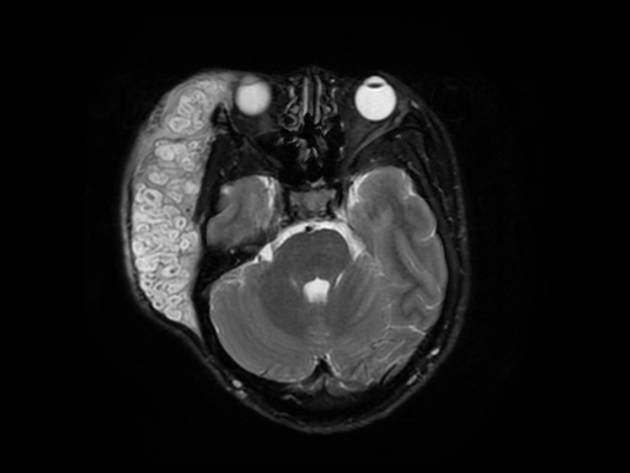
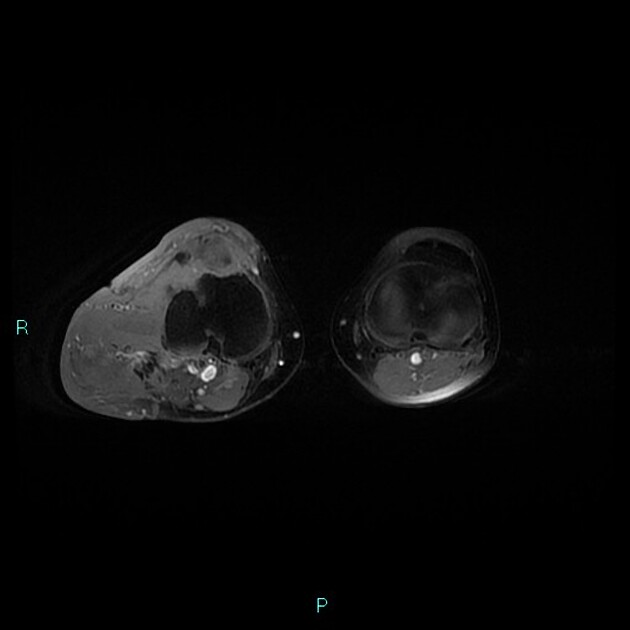
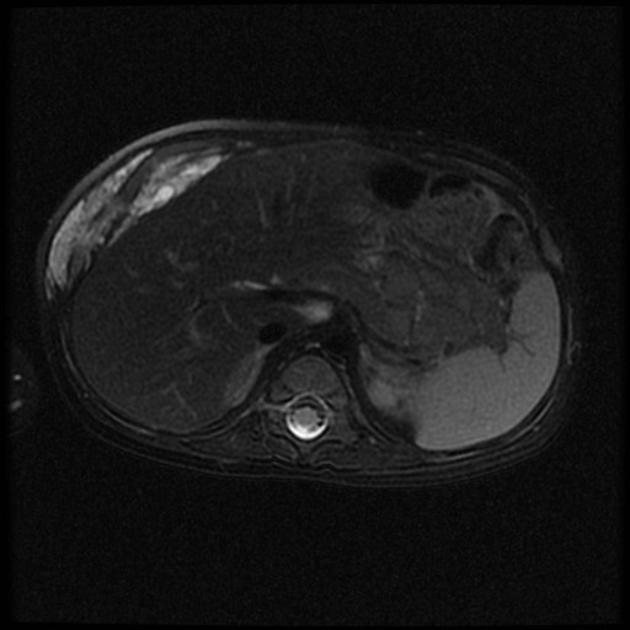
MRI
Reported signal characteristics include:
T1: hypointense
T2: hyperintense +/- hypointense central focus (target sign)
T1 C+: mild enhancement
Surveillance
The mode and frequency of surveillance for patients with NF1 but without diagnosed optic pathway gliomas varies depending on local preference and resources. The European Reference Network on Genetic Tumour Risk Syndromes (ERN GENTURIS) 2023 guidelines suggest the following 7:
clinical assessment for plexiform neurofibromas should begin at diagnosis or birth and be carried out at every clinical visit by clinicians with NF1 expertise, using observation, palpation, and neurological examination; photography or video can be useful adjuncts to these assessments
imaging by whole-body MRI should be performed at least during the transition from childhood to adulthood predict the risk of future malignant peripheral nerve sheath tumour (MPNST) based on internal tumour burden
if no internal plexiform neurofibromas are detected at this time, only clinical assessment is required
if internal plexiform neurofibromas are detected then periodic repeat imaging should be performed based on local preference and guided by a multidisciplinary team
symptomatic plexiform neurofibromas would be monitored more frequently ideally with FDG PET-MRI if available, or failing that then FDG PET-CT
Treatment and prognosis
Although generally benign tumours, there is a significant potential for malignant transformation, which occurs in 5-10% of larger tumours 5,6. If complete resection is possible, then a cure can be effected, however, due to the infiltrating nature of these tumours, such a resection is usually not possible. In such cases MEK inhibitors can be considered 7.
History and etymology
The term plexiform comes from the infiltrative growth pattern that, histologically, looks like a plexus or a network. Plex- originates from the Latin verb plectere meaning "to plait" or "interweave".
It is typically associated with tumours of neural derivation. Plexiform neurofibromas are considered the prototype of the plexiform pattern 1.
Differential diagnosis
On imaging consider:










 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.