Re-expansion pulmonary edema is an uncommon but important cause of non-cardiogenic pulmonary edema.
On this page:
Clinical presentation
Pulmonary edema occurs in the setting of rapid re-expansion of a collapsed lung, presenting as acute dyspnea. The onset can be delayed by up to 24 hours. It occurs following ~1% of pneumothorax re-expansions or thoracentesis procedures and mortality has been reported at 20% 7. Re-expansion pulmonary edema has also been reported following non-pulmonary procedures, such as hepatic cyst drainage with consequent re-expansion of atelectatic lung 1.
Pathology
The exact underlying mechanism is unknown but is thought to be a form of permeability edema 4 related to endothelial changes occurring when the lung has been collapsed for 3 or more days. Hydrostatic edema may be a contributing factor in some cases 5. High negative intra-pleural pressure may be a risk factor.
Bilateral pulmonary edema can occur and is likely due to a combination of reperfusion injury and inflammatory response. In this scenario, the mortality rate can be as high as 40% 4.
Risk factors
Rapid lung re-expansion in the following settings 2:
rapid drainage of large pneumothoraces/pleural fluid collections
patients in whom the lung has been collapsed for over 7 days
Radiographic features
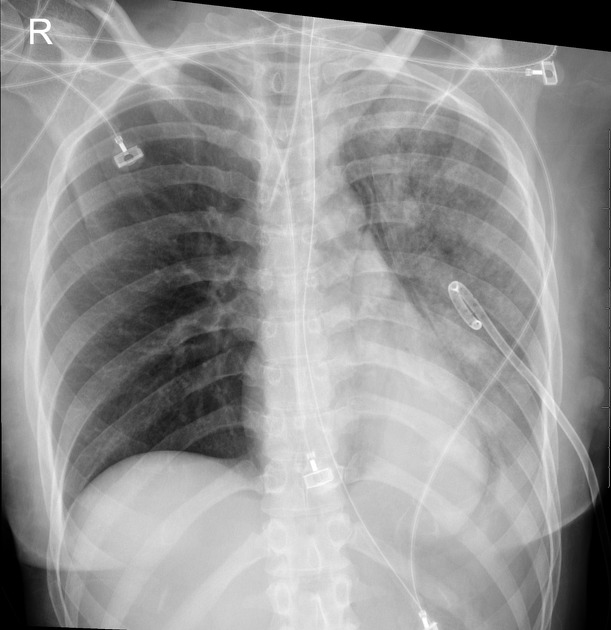
Plain radiograph
alveolar (air-space) opacity
usually unilateral in those portions of the lung that were previously collapsed
rarely edema can develop in the contralateral lung
the clinical setting is critical to making the diagnosis
edema may persist for several days and up to one week
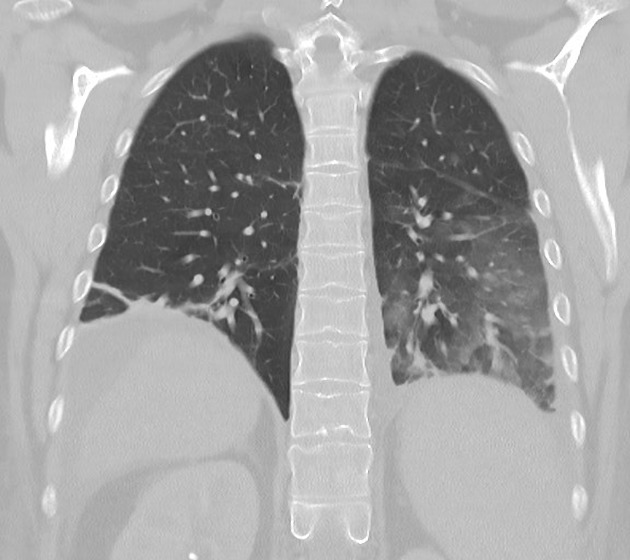
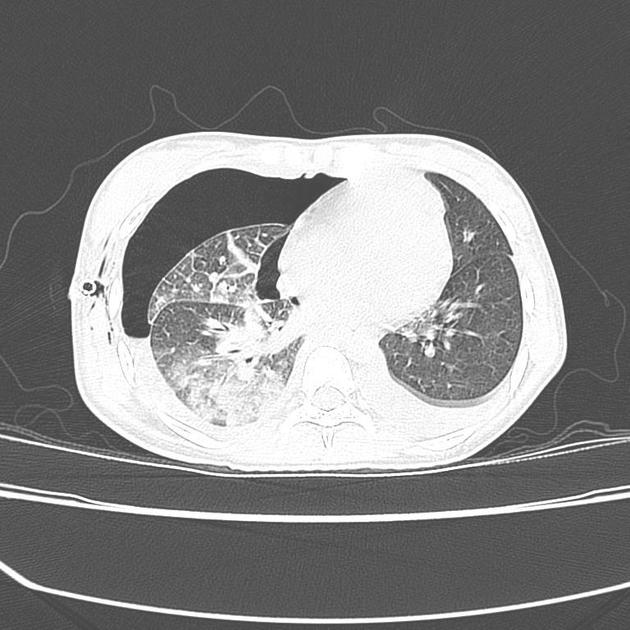
CT
Re-expansion edema appears as regions of ground glass opacification. It may be peripheral in distribution and associated with smooth interstitial thickening 3 however the distribution varies and dependent opacity along fissures and interlobular septa can occur.
Prevention
Pre-procedure checks will identify patients at risk and rapid re-expansion should be prevented by the use of clamps or taps.
Measured aspiration limited to 1-1.5L/hour is safer than an underwater seal for large sub-acute pneumothoraces.
Treatment
If respiratory distress occurs during drainage of a large pleural effusion, consider reintroducing the pleural fluid into the thoracic cavity. A report of two cases indicates rapid resolution of symptoms 6.







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.