Seminal vesicle cyst
- Integral Diagnostics, Shareholder (ongoing)
- Micro-X Ltd, Shareholder (ongoing)
Updates to Article Attributes
Seminal vesicle cysts can be congenital or acquired.
Epidemiology
Age of presentation of congenital seminal vesicular cysts is during the period of greatest reproductive activity i.e. in second and third decades of life, while acquired cysts are most often seen in the elderly age group.
Clinical presentation
Smaller cysts may be detected incidentally. In symptomatic patients, the usual presenting features include perineal pain, abdominal pain, ejaculatory pain, dysuria, haematuria, increased frequency of micturition, urinary tract infections and infertility.
Pathology
Aetiology
Congenital
Congenital cysts occur due to insufficient drainage as a result of atresia of the ejaculatory ducts causing distension of seminal vesicles and further leading to the formation of a cyst. They usually become symptomatic in young adulthood due to the accumulation of secretions. These cysts are mostly unilateral with no predilection for the side of involvement.
Congenital cysts are associated with many other urogenital anomalies:
renal dysgenesis (includes renal agenesis) 1
ectopic insertion of ureter into seminal vesicle, ductus deferens, ejaculatory duct or prostatic urethra
Acquired
Acquired cysts are seen most often secondary to prostatic infection or surgery causing scarring and finally obstruction of the drainage of secretions. This is seen most often bilaterally.
obstruction by benign prostatic hypertrophy
chronic infection and scarring of the seminal vesicle or ejaculatory duct
prior prostate surgery
Radiographic features
Seminal vesicles appear normal or enlarged in size with presence of cysts within.
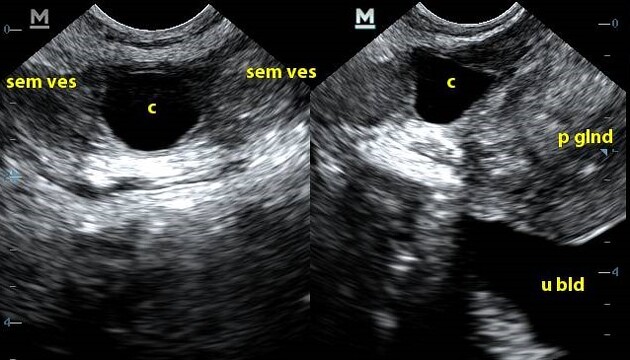
Ultrasound
These can be imaged by transabdominal ultrasound and are best evaluated by transrectal ultrasound. The cysts may be anechoic or may contain internal debris from haemorrhage or infection.
CT
Larger cysts may be seen on CT. The cysts may be seen as well defined, low attenuation lesions or thick and irregular walled cysts with hyperdense contents in cases of secondary haemorrhage or infection. These lesions are classically located in the retrovesicular region and cephalic to prostate. The associated renal anomalies can be depicted well.
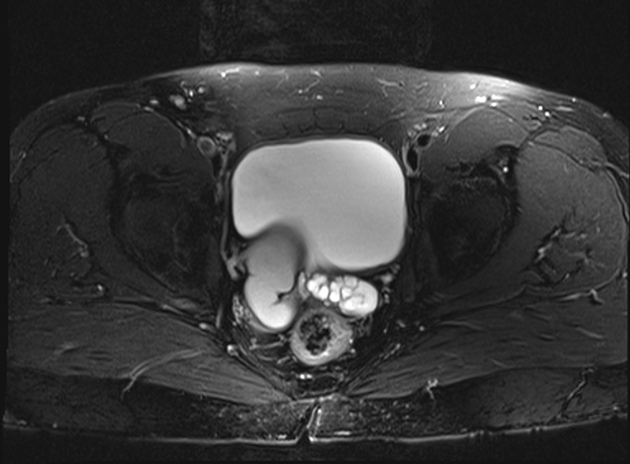
MRI
Best in differentiating cystic pelvic lesions. Abdominal and pelvic anatomy can also be assessed. Classical appearance of cysts is maintained with low T1 and high T2 weighted signal intensity. Some seminal vesicle cysts may have high T1 and T2 signals probably due to proteinaceous contents or haemorrhage.
Treatment and prognosis
Depending on the size of the seminal vesicle cyst, surgery may be helpful.
Differential diagnosis
Other causes of male pelvic cystic masses can be included as a differential diagnosis.
Müllerian duct cyst
-: usually midlineejaculatory duct cyst
-: usually midlinediverticulosis of ampulla of ductus (vas) deferens
-: lateral in location
See also
Image 5 Ultrasound ( create )








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.