Septo-optic dysplasia (SOD), also known as de Morsier syndrome, is a condition characterized by optic nerve/tract hypoplasia and absence of the septum pellucidum and, in two-thirds of patients hypothalamic-pituitary dysfunction. It is best thought of as being part of the holoprosencephaly spectrum (see classification system for midline malformations).
On this page:
Epidemiology
Septo-optic dysplasia has an estimated prevalence of ~1:50,000. There is no recognized gender predilection.
Risk factors
A number of risk factors have been identified 8,9:
maternal diabetes
-
medications
quinidine ingestion
antiseizure medications
drug and alcohol use
cytomegalovirus infection
Clinical presentation
Clinical presentation of septo-optic dysplasia is varied and mostly dependent on whether or not it is associated with schizencephaly (~50% of cases). This association is used to define two forms of the condition 1,8:
-
not associated with schizencephaly
visual apparatus more severely affected
hypothalamic-pituitary dysfunction present in 60-80% of patients 6,8
may present as hypoglycemia in the neonatal period 6
small pituitary gland with hypoplastic or absent infundibulum and ectopic posterior pituitary seen as a focus of T1 high signal intensity in the median eminence of hypothalamus
olfactory bulbs may be absent (arhinencephaly) 8
-
associated with schizencephaly
optic apparatus less severely affected
cortical anomalies: polymicrogyria, cortical dysplasia
may be etiologically different 8
sometimes referred to as septo-optic dysplasia plus 8
In addition, a number of other associations are recognized including:
Pathology
The abnormality develops during 4th-6th weeks of gestation, during early forebrain development. The exact etiology is unknown, with an underlying genetic defect currently accounting for <1% of cases 9.
Radiographic features
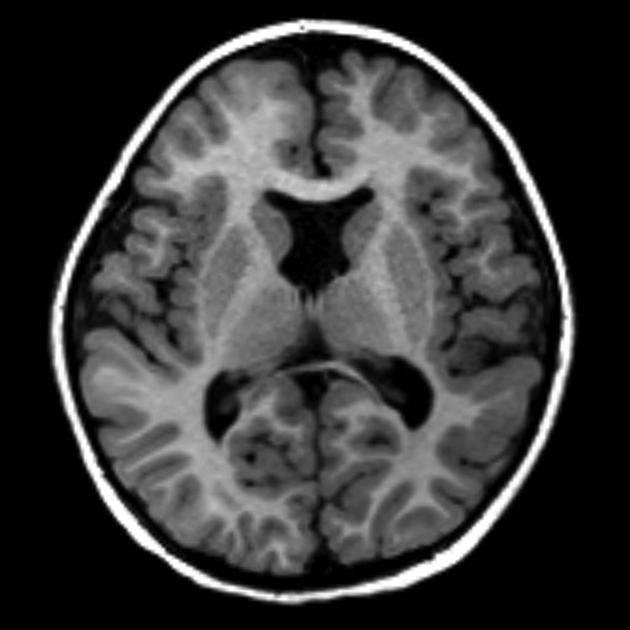
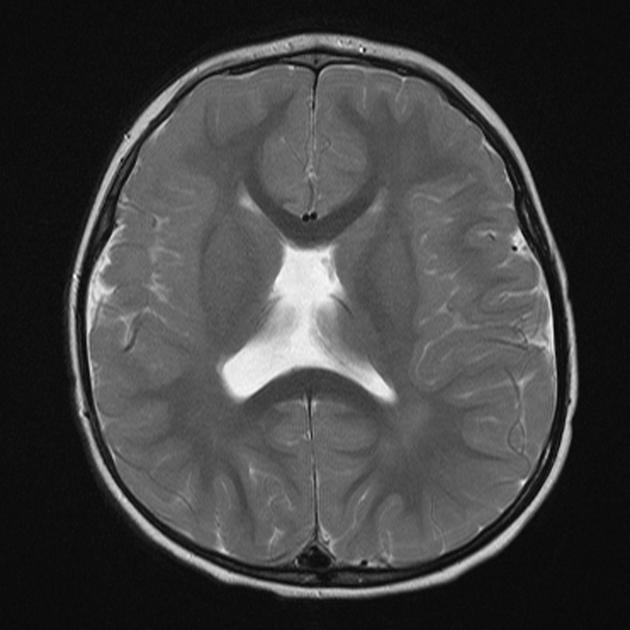
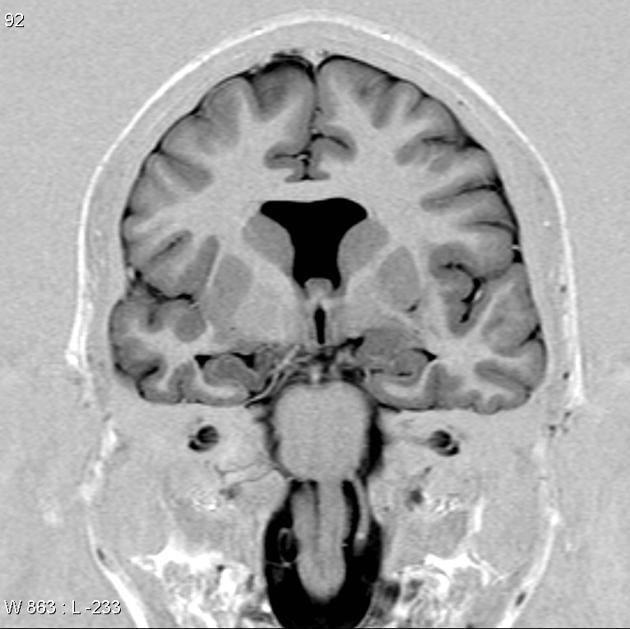
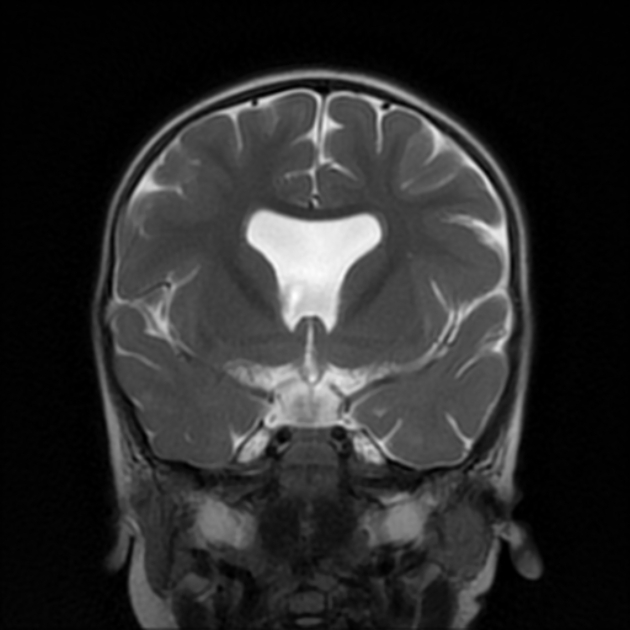
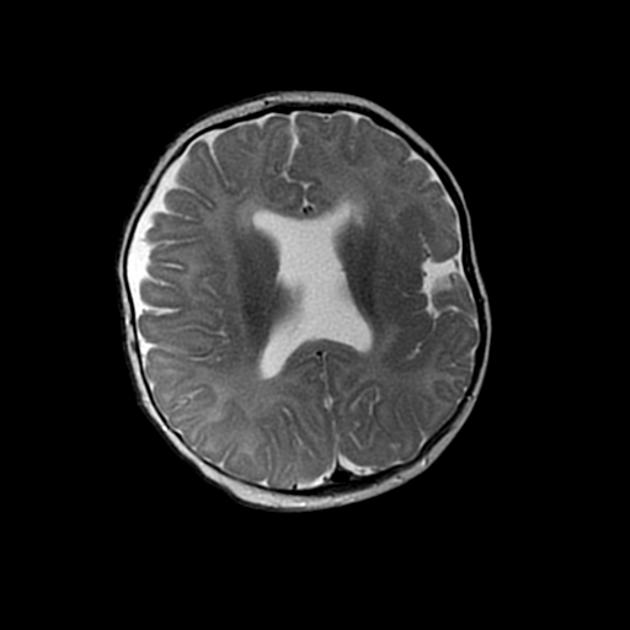
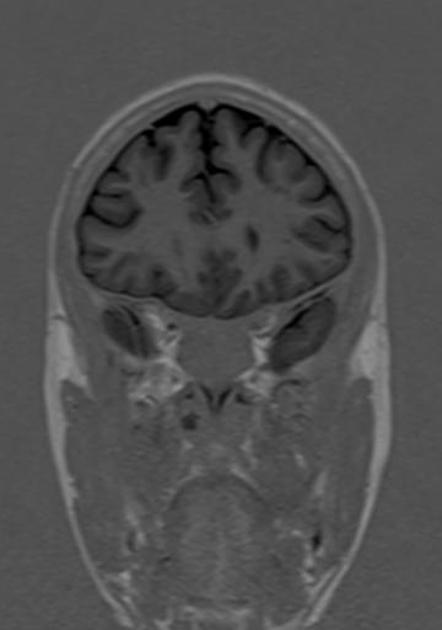
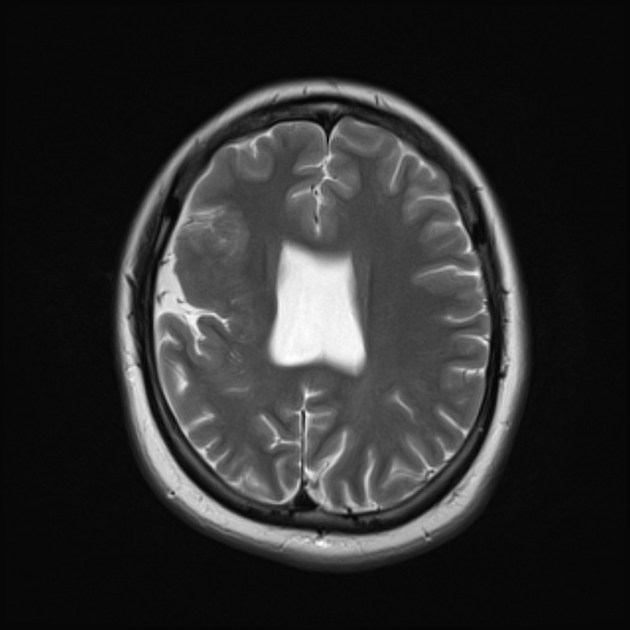
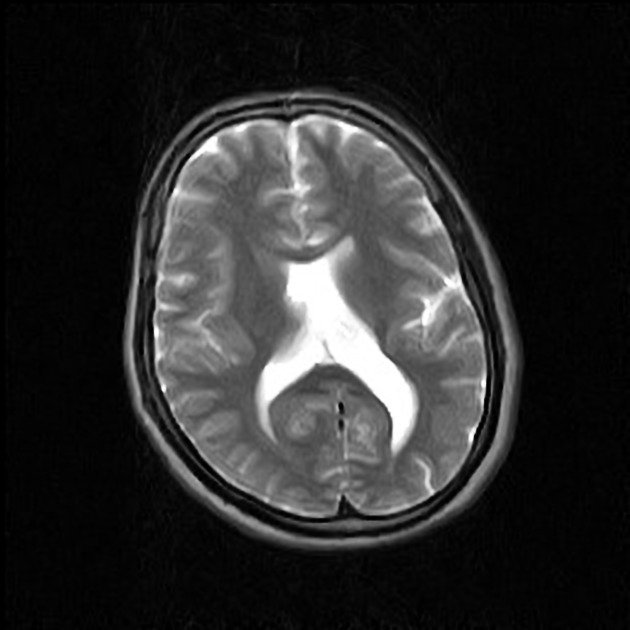
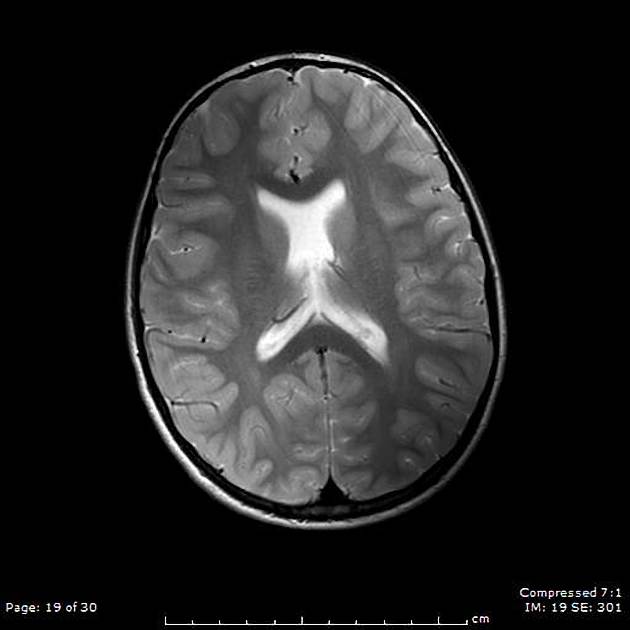
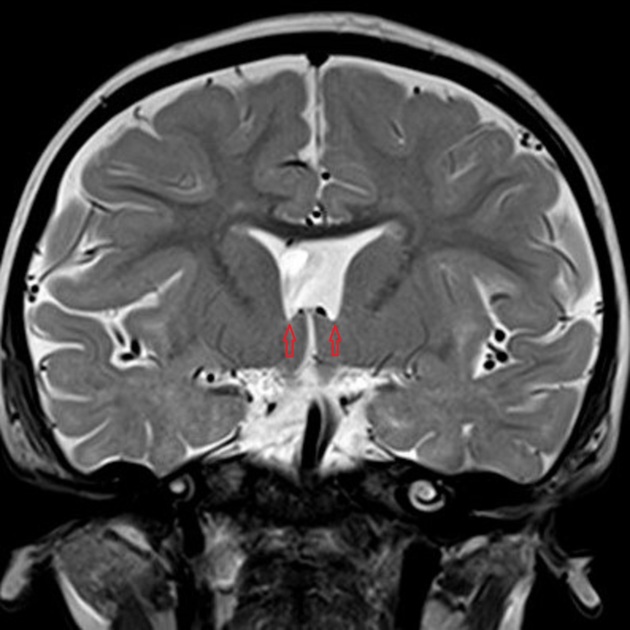
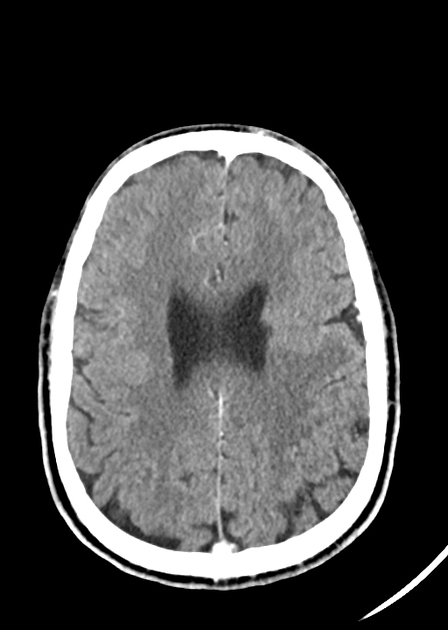
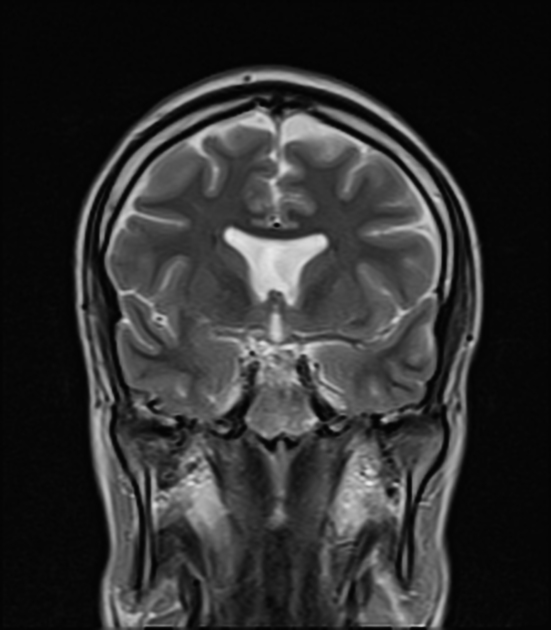
All imaging modalities that can visualize the septum pellucidum (ultrasound, CT and MRI) will detect its absence in septo-optic dysplasia. Some additional modality dependent features may also be visible.
CT
In addition to enlarged lateral ventricles with an absent septum pellucidum, CT may demonstrate small optic apparatus (best seen with volumetric scanning and coronal reformats) and associated small bony optic foramina.
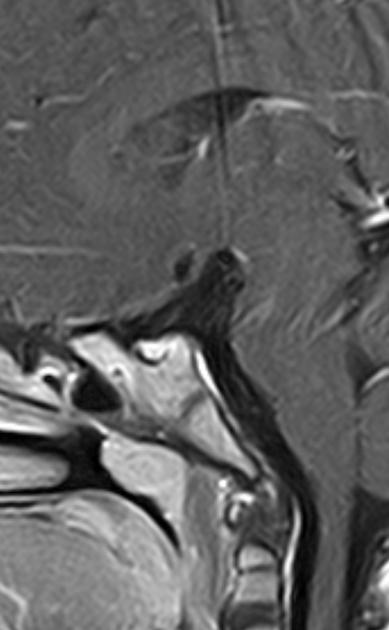
MRI
MRI is the modality of choice for assessing septo-optic dysplasia.
may show a "point down" appearance of the lateral ventricular frontal horns on coronal images
absent septum pellucidum
hypoplastic pituitary stalk
hypoplastic optic chiasm/optic nerves and globes
Treatment and prognosis
The management of septo-optic dysplasia requires a multidisciplinary team to assess and treat for hormonal imbalance, loss of vision, autism and obesity 9.
History and etymology
Septo-optic dysplasia was first described by George de Morsier (1894-1982), Swiss neurologist in 1956 6,7.
Differential diagnosis
Consider
-
may not be able to be differentiated 8
anterior cerebral artery will have its course shifted anteriorly in lobar holoprosencephaly (sign described on prenatal ultrasound also, midline sagittal view with color Doppler)
optic chiasm is not expected to be hypoplastic







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.