Spinal arteriovenous malformations (AVMs) are characterized by arteriovenous shunting with a true nidus. They represent ~25% of spinal vascular malformations.
On this page:
Epidemiology
Different types of spinal AVM have different ages of presentation, but overall 80% present between the age of 20 and 60 years 3.
Clinical presentation
Clinical presentation is variable, ranging from progressive myelopathy (Foix-Alajouanine syndrome), often with delayed diagnosis, to catastrophic spinal subarachnoid hemorrhage (see: coup de poignard of Michon 3).
Pathology
Classification
Spinal AVMs can be classified into:
compact intradural intramedullary glomus AVM (type II)
mixed extradural-intradural intramedullary juvenile AVM (type III)
For a detailed description of alternative classification systems, see:
Radiographic features
Angiography (DSA)
Angiography remains the investigation of choice but requires meticulous technique. It is essential to remember that the site of arterial supply can be anywhere from the upper thoracic to sacral areas with little relationship to the clinical level, or visible nidus (if present).
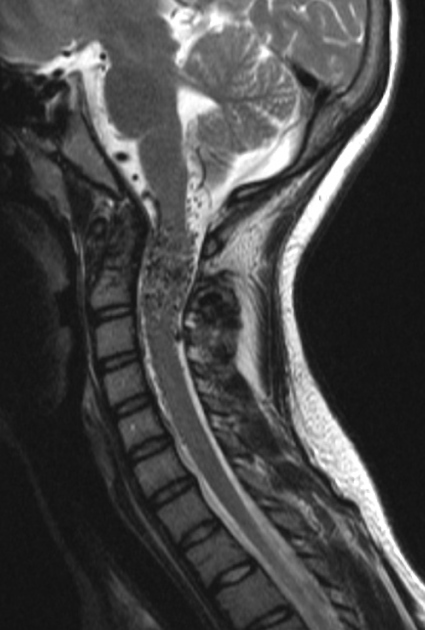
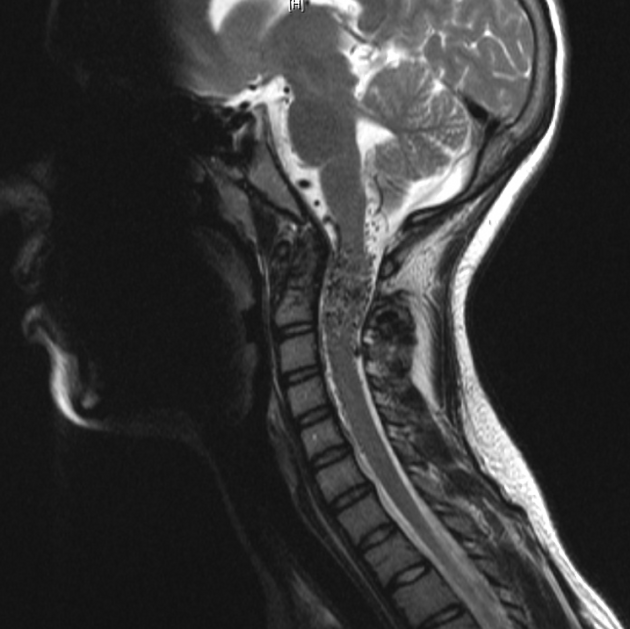
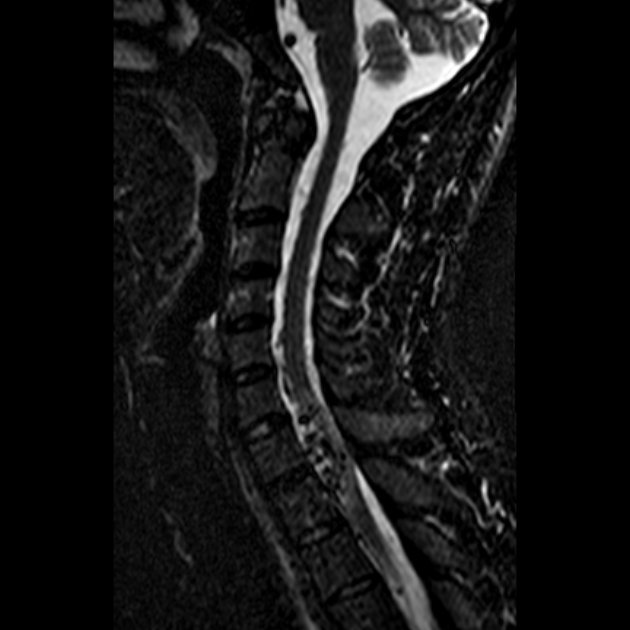
MRI
-
T1
signal voids from high-velocity flow
dilated perimedullary vessels indent/scallop the cord 1
-
T2
signal voids from high-velocity flow 1
increased cord signal due to cytotoxic edema or myelomalacia 1
Treatment and prognosis
Both surgery and angioembolisation have a role in the treatment of spinal AVMs 6.
Complications
myelopathy from venous congestion/hypertension
hemorrhage: within the cord parenchyma or subarachnoid space 6
high-flow AVMs may cause arterial steal from adjacent spinal cord segments 6
myelopathy from large AVMs (rare) 6







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.