Neurenteric cysts (also sometimes spelled neuroenteric) are developmental lesions arising from endoderm, most commonly encountered in the spinal canal but also seen in the posterior fossa and more rarely, supratentorially.
On this page:
Epidemiology
Although congenital, presentation is usually delayed until late childhood or early adulthood 4, presumably due to slow accumulation of cyst content. There is a 2:1 male predilection 4.
Clinical presentation
Clinical presentation varies widely depending on the location of the cyst.
Spinal neurenteric cysts present with symptoms and signs referable to the level of the cyst. This includes pain, weakness and paresthesias 4.
Intracranial neurenteric cysts tend to present with headache or cranial nerve deficits, although paresthesia, weakness, gait impairment, and seizures are all reported 3.
Pathology
They result from incomplete resorption of the neurenteric canal, a temporary connection between the yolk sac and amnion during early embryogenesis. They are usually solitary with only the occasional case report describing multiple cysts at diagnosis 4,7.
Macroscopic appearance
Neurenteric cysts have a relatively thick outer wall enclosing fluid that is of variable appearance and consistency, ranging from serous CSF-like fluid to thicker jelatinous or mucionus fluid. Color is also variable ranging from clear to opaque and white to near-black 4.
Microscopic appearance
The cyst wall can vary in composition, typically containing either columnar or cuboidal cells, with or without cilia. Additional components of various types may be encountered, including cartilage, fat, bone, lymphatic tissue, fat, glandular components, ependymal or glial tissues 4. Mucin production is variably present 4.
Location
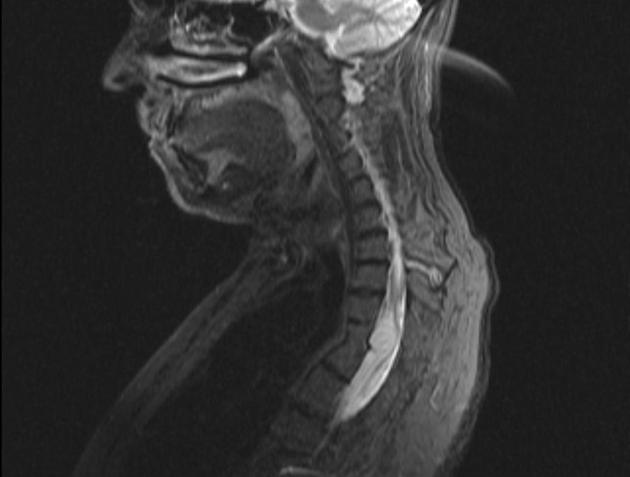
Neurenteric cysts are extra-axial. Approximately 75% of all neurenteric cysts are located in the spinal canal 3.
The intraspinal cysts are usually intradural extramedullary (80-90%) 4 and ventral in location 5. Only rarely are they intramedullary or extradural 4. They most commonly occur in the thoracic region (~40%).
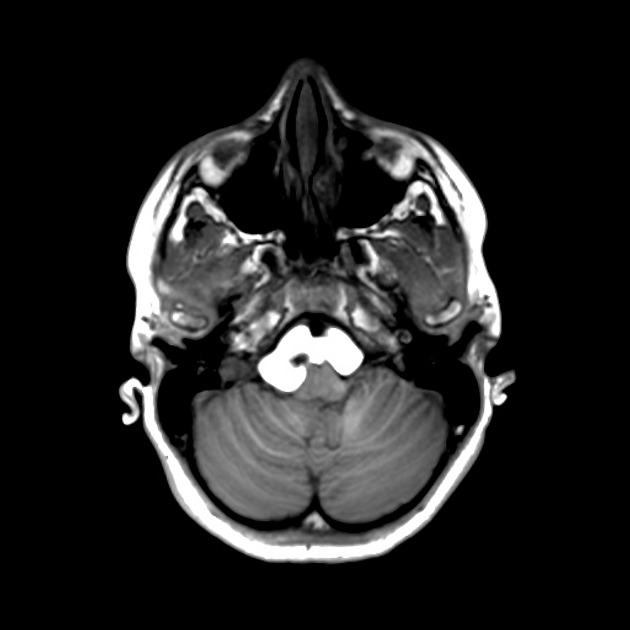
When located in the intracranial compartment, 80% of cases are in the posterior fossa, usually anterior to the pontomedullary junction although other locations are described including within the fourth ventricle 1. The remaining 20% are located in the supratentorium, most commonly adjacent to the central base of skull (e.g suprasellar or parasellar) or in the anterio cranial fossa 1,3.
Associations
vertebral anomalies like Klippel-Feil syndrome, hemivertebra, butterfly vertebra, scoliosis, split cord and spina bifida 5,6
Radiographic features
CT
On CT, neurenteric cysts vary in density ranging from fluid-like density similar to CSF, to isointense to brain parenchyma to hypderdense 1,3. They usually demonstrate no enhancement, although rarely minor wall enhancement may be seen 1.
MRI
MRI is the modality of choice, and appearances depend on the variable protein content 1-4:
T1: variable, ranging from isointense to CSF to very high T1 signal (white)
T2: variable, ranging from isointense to CSF to very low T2 signal (black)
FLAIR: T2 high signal lesions do not suppress on FLAIR 3
DWI/ADC: ranging from mild diffusion restrion to facilitated diffusion 1,3
Differential diagnosis
Imaging differential considerations include:
-
similar to CSF in signal
high DWI signal, ADC similar to brain parenchyma
-
CSF signal on all sequences
-
solid enhancing component
-
fat signal on all sequences
suppression on fat-suppressed sequences
-
a stalk-like connection to the clivus
variable enhancement
-
usually enhances following IV contrast




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.