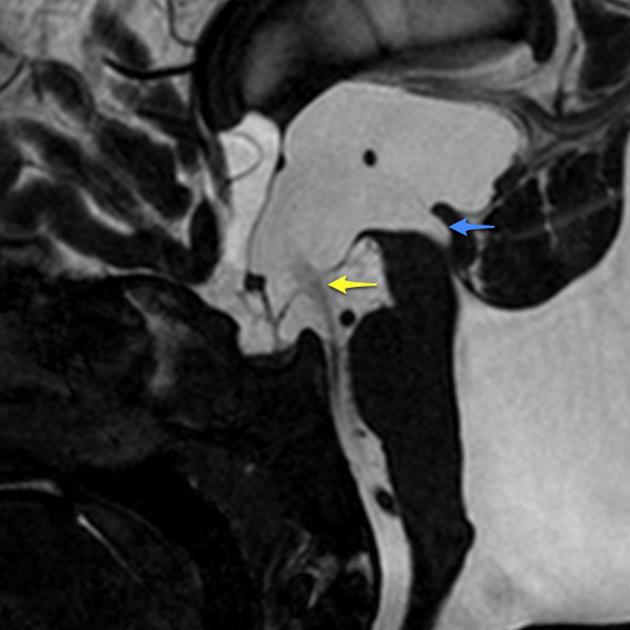
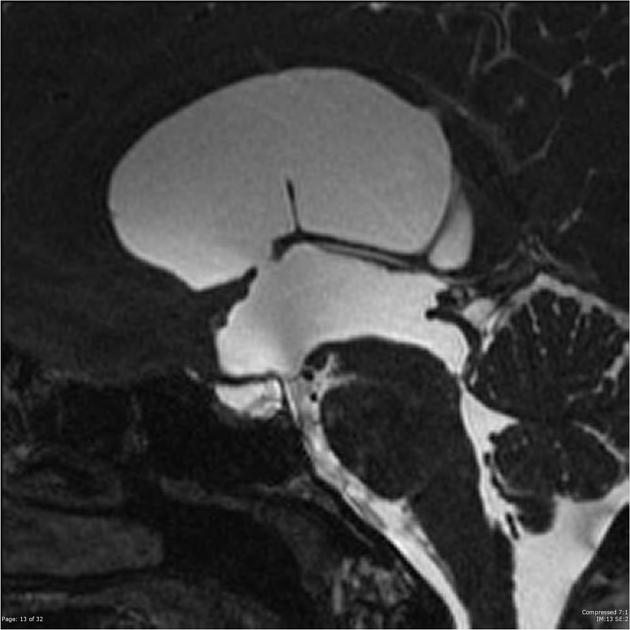
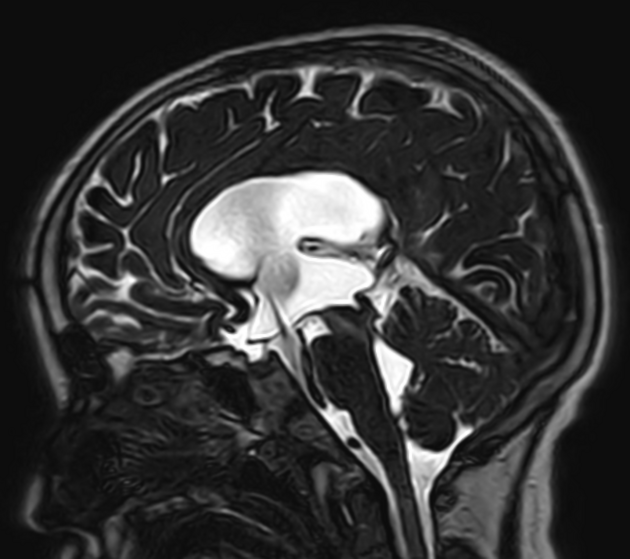
A third ventriculostomy is a type of surgical treatment for obstructive hydrocephalus, especially when obstruction is located at the level of the aqueduct of Sylvius (e.g. aqueduct stenosis). A permanent defect is created in the floor of the third ventricle anterior to the mammillary bodies, thus connecting the third ventricle with the interpeduncular cistern.
Follow up MRI studies may be necessary to confirm patency. This can be directly visualized on high resolution T2 weighted sagittal imaging and/or by performing CSF flow studies.
Complications
Hydrocephalus may develop after a successful third ventriculostomy secondary to several reasons, despite initial relief provided by the procedure, such as 3-5,:
closure or scarring of the stoma: over time, the surgical created opening (stoma) may close due to fibrosis or scarring which could be caused by inflammation, infection or individual healing response 3
inadequate stoma size: if the stoma created was too small or not properly positioned 4
development of communicating hydrocephalus: impaired CSF absorption at the arachnoid granulations will cause communicating hydrocephalus which will not be alleviated by a third ventriculostomy 3
suboptimal flow dynamics: even with a patent stoma, CSF dynamics may not fully normalize due to altered pressure gradients or insufficient drainage of CSF into the subarachnoid space 5
progression of aqueductal stenosis: as the aqueductal stenosis itself may worsen contributing to increased CSF accumulation despite the ventriculostomy 5
new obstruction or secondary factors such as the development of postoperative adhesion in the subarachnoid pathways 3
History and etymology
First developed in the early 1900s prior to advent of VP shunting, and at that time employed a subfrontal approach with sacrifice of the optic nerve! In 1923 a urologist by the name of William Mixter used a urethroscope to perform the first endoscopic ventriculostomy.






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.