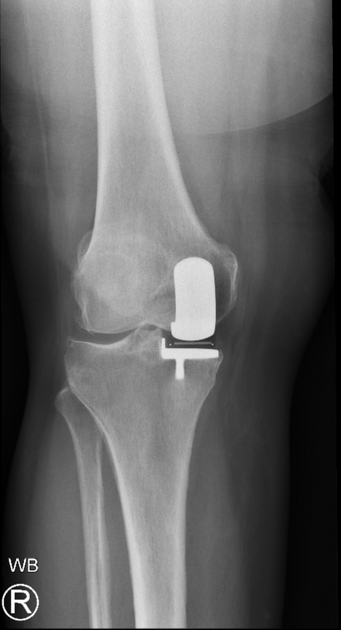
Total knee arthroplasty (TKA), total knee replacement (TKR), or tricompartmental knee replacement is an orthopedic procedure whereby the three articular surfaces of the knee (femoral, tibial, and patellar) are replaced by prosthetic components.
TKA is the most common joint arthroplasty performed in the United States, with an estimated 672,000 TKAs performed in 2009. Interestingly, the rate of knee arthroplasty for females was 57 % higher than for males 1.
On this page:
Indications
The most common indications for TKA include:
debilitating osteoarthritis
trauma/fracture
Contraindications
Contraindications to TKA include:
Prosthesis design
tibial component: high-density polyethylene spacer
femoral component: metallic component, surfaces contoured similarly to the femoral condyles and trochlea
patellar component: high-density polyethylene; may be metal-backed
Most designs use polymethylmethacrylate (PMMA) cement for fixation. Cementless designs are available, where fixation is achieved initially by friction, then by ingrowth of bone into the prosthesis.
There are many designs in use, but broadly speaking, TKA is characterized by the degree of constraint, polyethylene spacer fixation, and posterior cruciate ligament (PCL) retention or removal.
Degree of constraint
unconstrained prostheses: most widely used; the patient's supporting soft tissues help maintain stability
semi-constrained implants: more stable, decreased range of motion; closely conforming tibial and femoral components
-
constrained implants: hinged mechanism; most stable, but most limited range of motion, meaning more mechanical stress and susceptibility to wear, fatigue, and loosening; usually used in:
revision arthroplasty
elderly patients with highly unstable ligaments
combination with tumor resection
Spacer fixation
fixed bearing: the tibial spacer is fixed in a metal tibial tray
mobile bearing: a mobile polyethylene insert glides along the surface of the metallic tibial component
PCL retention vs removal
The PCL, an important knee stabilizer, can be:
retained; this is usually the case with unconstrained prostheses
removed
removed and substituted for by a PCL-substituting mechanism in the prosthesis
The decision whether to retain or remove the PCL depends mostly on the surgeon's preference and experience.
Radiographic features
Plain radiograph
The most cost-effective and commonest method of follow-up. Baseline radiographs should be obtained immediately post-operation.
Normal appearance on routine views:
-
AP
mechanical axis corrected to 0 degrees, results in femoral component placed 5-9 degrees valgus to long axis of femur 3
tibial component: aligned perpendicular to long axis of tibia
polyethylene (radiolucent) spacer in tibiofemoral joint space: equal width medially and laterally; NB: beam angle, patient positioning or post-op flexion contracture may distort this
-
femoral component: perpendicular to long femoral axis, unless surgeon has chosen to flex component by up to 3 degrees
tibial component: perpendicular to long tibial axis or posteriorly inclined by up to 5 degrees
patella: anterior and articular sides parallel to each other. Oblique patella on true lateral view suspicious for subluxation, patella alta for patellar tendon rupture, and significant patella baja for quadriceps tendon rupture
-
for assessing patellofemoral alignment: patellar component should be centered above femoral component trochlea
CT and MRI
True axial imaging allows assessing for rotational alignment of the femoral component. To this end, two lines are drawn, which should be parallel:
transepycondylar line, or axis: drawn between the sulcus of medial epicondyle and peak of the lateral epicondyle
a second line is drawn across the posterior margins of the femoral component
if the lines diverge medially, the component is externally rotated: can cause an increased medial flexion gap and result in flexion instability
if they diverge laterally, the component is internally rotated: early or delayed patellofemoral complications may ensue, especially if internal rotation exceeds 5 degrees
Complications
The 15-year endurance for knee prostheses is 95%, owing to advances in prosthetic design and surgical technique. However, several there are several potential complications of knee arthroplasty:
-
most common complication
can occur up to 20 years post implant
tibial component more commonly affected than the femoral component
pain: up to 20% of patients have more pain/swelling than pre-replacement 11
-
instability due to ligament injury or implant malposition/failure 11
knee dislocation is rare 11
arthrofibrosis: ~5% (range 3-10%) 11
-
anterior knee pain: ~20% (range 8-30%) of patients 9,10
functional pain from pre-operative quadriceps muscle weakness 9
patellofemoral instability (maltracking rather than dislocation): in ~1% 8-11
patella baja (uncommon) 9
progressive chondromalacia in an unsurfaced patella 9,11








 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.