Transient synovitis of the hip refers to a self-limiting acute inflammatory condition affecting the synovial lining of the hip. It is considered one of the most common causes of hip pain and limping in young children. Over 90% of hip joint effusions in children tend to be due to transient synovitis 10.
On this page:
Epidemiology
It typically affects young children (3-8 years of age). There is a recognized increased male predilection.
Clinical presentation
Patients typically present with hip pain for one to three days, associated with limping or the refusal to bear weight.
Pathology
Their exact pathogenesis is not well known. Several theories have been proposed. In some situations, it may follow an upper respiratory tract infection. Some have suggested a viral etiology; potentially related to Parvovirus B19 and/or herpes simplex virus 6 infections. Others have proposed a post-traumatic etiology with subsequent development of chemical synovitis.
Radiographic features
Plain radiograph
Features are nonspecific although in some cases there may be an increase in medial joint space in the affected hip 5. Hip radiography within 6 months (classically after 4 weeks) to exclude Legg-Calvé-Perthes (LCP) disease is recommended 12.
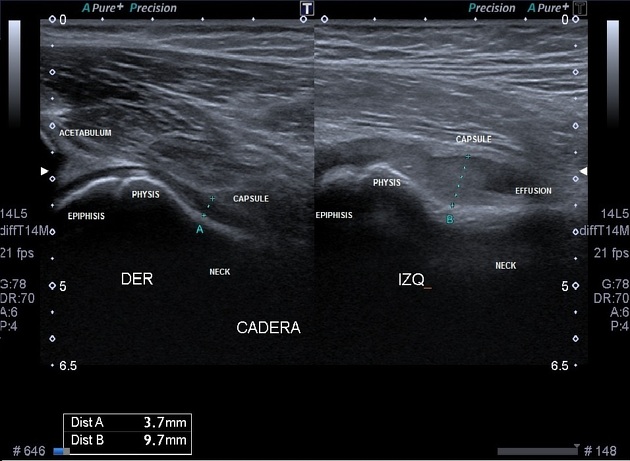
Ultrasound
Ultrasound is useful for demonstrating a joint effusion which is often seen in the anterior recess. Herniation of the synovial membrane through a joint capsular defect (pseudodiverticulum) between the iliopsoas muscle and the anterior border of the joint capsule may be seen in a very small proportion of patients (~2%) 1.
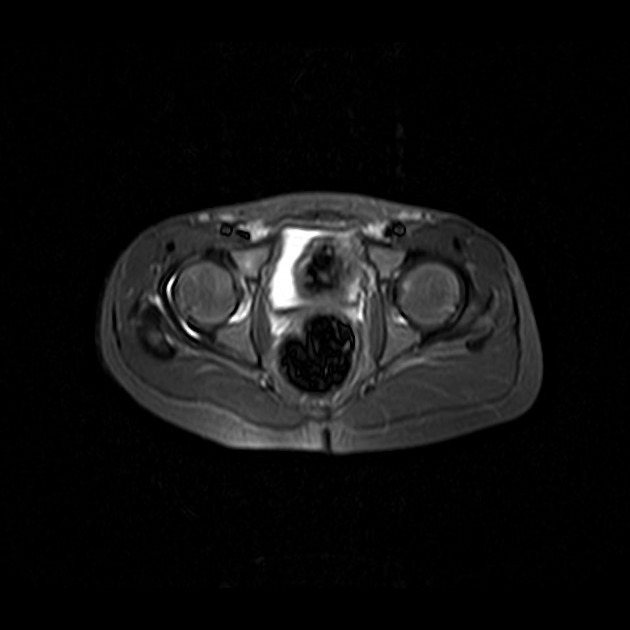
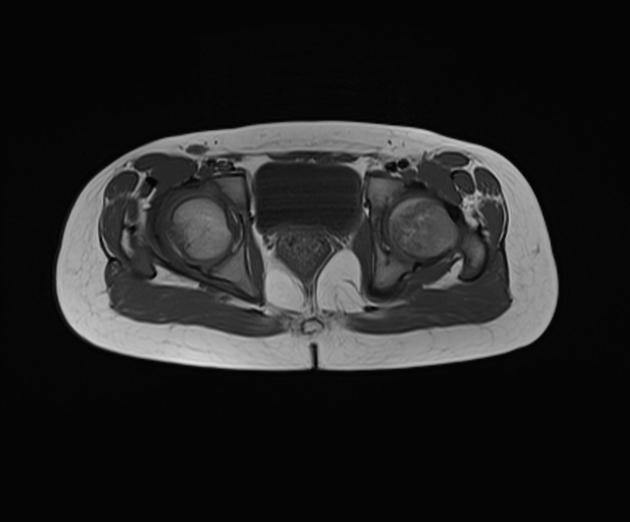
MRI
Described features include 6:
symptomatic hip joint effusion
contralateral joint effusion
signal alterations and enhancement in surrounding soft tissue
usually no signal alteration in the adjacent marrow
Treatment and prognosis
It is a self-limiting disorder that usually has no residual sequelae. Recurrence is possible. Management is usually supportive.
Differential diagnosis
For imaging appearances, possible considerations include:
septic arthritis: on MRI there is often signal abnormality in marrow 8, and classically affects children "younger than 4 years and with a history of fever" while it is "older than 4 years of age and no history of fever" for transient synovitis 11; the Kocher criteria could also be used to aid in differentiating these diagnoses 14
For clinical limping, there is a much wider differential including other childhood arthritides (e.g. juvenile rheumatoid arthritis 1, Brucella arthritis), Perthes disease, epiphysiolysis, osteoid osteoma, etc.






 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.