The urinary bladder (more commonly just called the bladder) is a distal part of the urinary tract and is an extraperitoneal structure located in the true pelvis 6. Its primary function is as a reservoir for urine.
On this page:
Gross anatomy
The bladder has a triangular shape with a posterior base (fundus), superior dome, anterior apex, and an inferior neck with two inferolateral surfaces 6. It is lined with a rough, trabeculated transitional cell epithelium, except at the trigone 6.
The apex of the bladder is directed behind the symphysis pubis 6, connected to the anterior abdominal wall and umbilicus through the median umbilical ligament (remnant of the embryological urachus) 6, which is covered by the median umbilical fold formed by the overlying peritoneum.
The trigone is a triangular area of smooth mucosa lined by stratified squamous epithelium on the internal surface of the base. The superolateral angles are formed by the ureteric orifices and the inferior angle is formed by the internal urethral orifice.
As men age, the trigone overlying the mid-portion of the central zone of the prostate may start to protrude as the prostate enlarges forming a mild hemispherical elevation proximal to the internal urinary sphincter, which is called the uvula of the bladder 5.
The urethra arises from the neck of the bladder and is surrounded by the internal urethral sphincter. The urethra is separated from the symphysis pubis by retropubic fatty space of Retzius 6.
As the bladder fills with urine it becomes ovoid and extends superiorly into the abdominal cavity 6. Contraction is facilitated by the detrusor muscle.
The peritoneum over the bladder is relatively loose except at the insertion points of the ureters at the posterior bladder and at the inferior bladder where the peritoneum condensed into pelvic fascia and attached to the pubic bone (pubovesical ligament in females and puboprostatic ligament in males), lateral walls of pelvis and rectum. This makes the inferior part of the bladder relatively fixed. In males, the peritoenum is reflected between the rectum and bladder to form the rectovesical pouch. In females, there are two reflections namely rectouterine pouch (pouch of Douglas) and vesicouterine pouch 6.
Arterial supply
upper part in both males and females: superior vesical artery
-
lower part:
males: inferior vesical artery
females: vaginal artery
All of which are branches from the anterior division of the internal iliac artery 4.
Venous drainage
male: vesical and prostatic venous plexus via similarly named veins to the internal iliac veins and internal vertebral veins
female: vesical and uterovaginal plexuses draining into the internal iliac veins
Lymphatic drainage
upper part: lymphatic vessels pass to external iliac lymph nodes
lower part: lymphatic vessels pass to internal iliac lymph nodes
Innervation
-
autonomic innervation from the vesical nerve plexuses (composed of sympathetic and parasympathetic nerve fibers)
sympathetic: reach the pelvic and subsequently the vesical plexus via hypogastric nerves (from the inferior mesenteric ganglion which in turn is supplied by the lumbar splanchnic nerves from the sympathetic lumbar outflow)
parasympathetic: reach the pelvic and subsequently the vesical plexus via pelvic splanchnic nerves (from the parasympathetic sacral outflow)
somatic innervation is via the pudendal nerves
the hypogastric, pelvic splanchnic and pudendal nerves all have afferent components
For an account of the functional anatomy of micturition, refer to bladder neuroanatomy. 2,3.
Relations - male
anteriorly: pubic symphysis
posteriorly: rectovesical pouch and rectum
inferiorly: obturator internus muscle, levator ani muscle, prostate (anterior to posterior) 6
superiorly: peritoneum
laterally: ischioanal fossa
Relations - female
anteriorly: pubic symphysis
inferiorly: urogenital diaphragm, pelvic fascia, perineal membrane
superiorly: uterus, peritoneum
laterally: ischioanal fossa
Variant anatomy
double bladder: receives ipsilateral ureter and has a separate urethra
septation: septum may divide the bladder internally into two or more compartments
agenesis: persistence of the cloaca
ureterocele: dilation of the intravesical part of the ureter
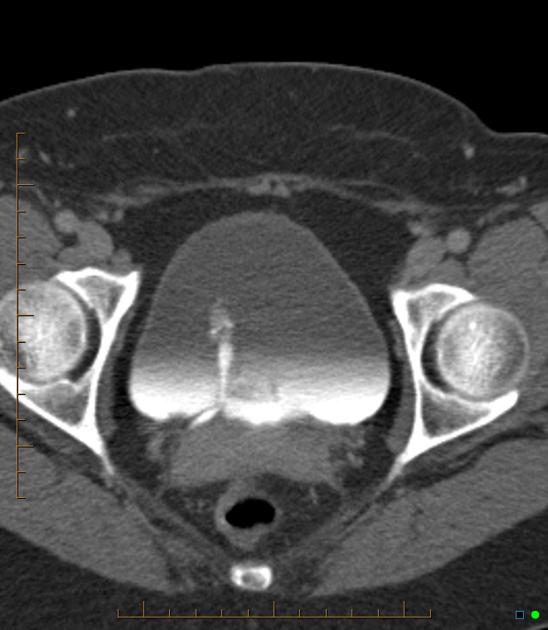
Radiographic features
The bladder is usually easier to evaluate when full, and it is sometimes difficult to identify when empty.
Plain radiograph
The bladder may be seen as a rounded soft tissue mass 1.
Fluoroscopy
Cystography can be performed where the bladder is filled with contrast either via an antegrade or retrograde technique.
Ultrasound
The bladder wall is best assessed with this modality - it should not exceed 3-5 mm in thickness. Ureteric jets can be assessed using color Doppler ultrasound 1.
MRI
T1: bladder wall and contents are homogeneous low signal
T2: bladder wall is of low signal and urine of high signal, allowing for a contrast between the two 1
Related pathology
-
signs
pine cone bladder or Christmas tree bladder
-
trauma
-
neoplastic
-
others







 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.