Presentation
Sudden onset of shortness of breath and tachypnea status post transfusion.
Patient Data
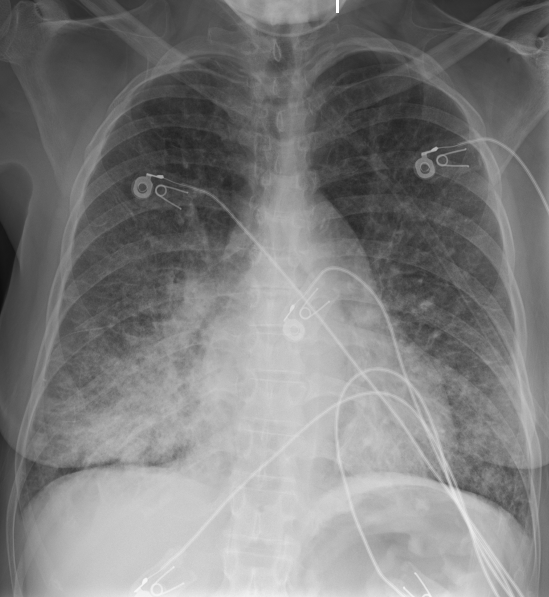
Moderate diffuse bilateral pulmonary vascular congestion and interstitial edema with diffuse bronchial wall thickening and Kerley B lines mainly in the mid and lower lung zones are compatible with pulmonary edema from transfusion associated circulatory overload given history of transfusion.
No discrete large effusion or pneumothorax. No discrete focal pneumonia.
Heart appears at upper limits normal with mild diffuse prominence of the main pulmonary artery.
No acute osseous findings. No free air in the upper abdomen.
Case Discussion
Patients presenting with shortness of breath and tachypnea immediately after transfusion should increase suspicion of pulmonary complications. With signs of increased pulmonary venous hydrostatic pressure such as pulmonary edema and pleural effusion, this case is most consistent with transfusion associated circulatory overload. Patients who develop transfusion associated circulatory overload have increased susceptibility to volume overload due to heart failure, renal dysfunction, hypoalbuminemia, or positive fluid balance.
This case was submitted with supervision and input from:
Soni C. Chawla, M.D.
Health Sciences Clinical Professor,
Department of Radiological Sciences,
David Geffen School of Medicine at UCLA.
Attending Radiologist,
Olive View - UCLA Medical Center.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.