Presentation
Abdominal pain. History of pancreatic divisum with chronic calcific pancreatitis.
Patient Data





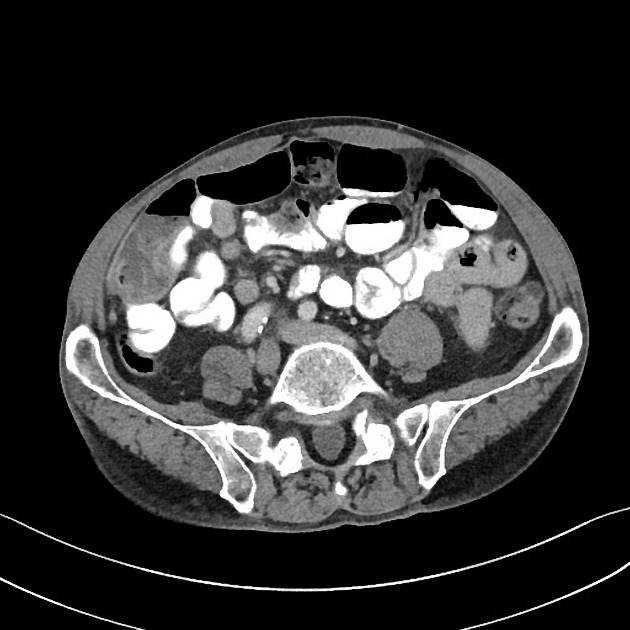
Severe low-attenuation submucosal thickening of the lower gastric body, antrum, and pylorus. Associated hyperemia of the gastric mucosa.
Common bile duct stent. Chronic calcific pancreatitis with dilatation of the pancreatic duct and multiple bulky intraluminal calcifications. No peripancreatic inflammation or fluid collections.
Case Discussion
Low-attenuation some mucosal thickening of the gastric wall is characteristic for severe gastritis or peptic ulcer disease. This may have been a reactive finding from subacute pancreatitis. This finding resolves on subsequent scanning and the patient did not undergo further intervention.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.