Presentation
Abdominal pain, diarrhea and bleeding per rectum. Raised D-dimer reaching 2700 ng/mL, Calprotectin 1448 ug/g.
Patient Data


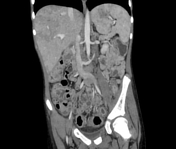



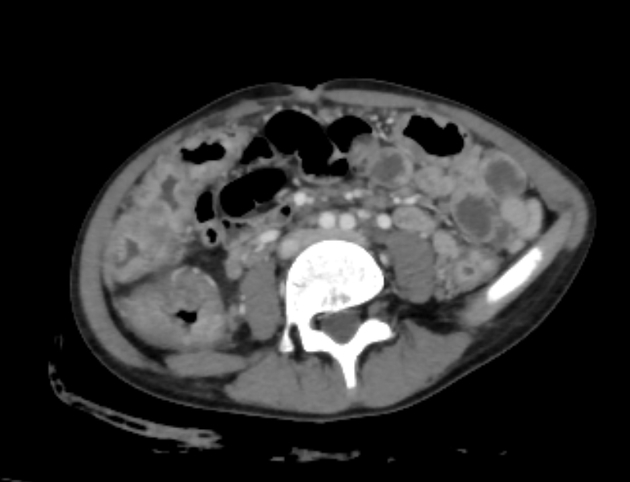
Large bowel shows pancolic involvement without skip lesions. Diffuse mucosal hyperenhancement starting from the rectum to the cecum with submucosal edema and congested vasa recta. Multiple mucosal ulcerations are noted. Diffuse stranding of inframesocolic omentum.
Small bowel shows normal mucosal enhancement and mural thickness. Multiple reactive mesenteric lymph nodes. Minimal free pelvic ascites. No pneumoperitoneum.
Multiple venous thrombi are noted at the right hepatic vein and its tributaries with mosaic perfusion of the related hepatic segments. Small non-occlusive thrombi are noted at one of the tributaries of the inferior mesenteric vein, left lumbar veins and left common iliac veins.

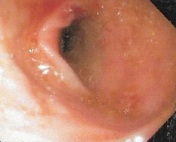








The colonic mucosa till the cecum is severely erythematous and edematous with absent vascular pattern. The mucosa is severely friable, granular, and covered by mucopurulent discharge with large pseudopolyps formation.
Conclusion: severe pancolitis. Biopsies were taken from ileum and rectosigmoid areas.
Pathology report
Pathologic diagnosis:
- endoscopic ileal biopsy: chronic active ileitis. This could represent backwash ileitis
- endoscopic colonic biopsies: inflammatory bowel disease, probably ulcerative colitis, negative dysplasia
Gross description: several grey white soft tissue fragments.
Microscopic examination:
Ileal bites: show an intact surface epithelial covering with mild villous blunting and focal erosions, an increase in number of lymphocytes infiltrating the surface epithelium is seen. The lamina propria shows moderate mixed acute and chronic nonspecific inflammatory cellular infiltrate. The inflammatory response is composed of lymphohistiocytic infiltrate with several eosinophils. Several grouped neutrophils are seen. No granulomata. No lymphoid hyperplasia is seen. A few reactive follicles are seen. The muscularis mucosa is not hypertrophic. The infiltrate doesn't affect the submucosa. An increase in number of lymphocytes infiltrating the surface epithelium is seen.
The colonic fragments: show n intact surface epithelium with a disrupted glandular architecture. The inflammatory gradient is lost. The lamina propria shows a moderate chronic nonspecific inflammatory cellular infiltrate. Typical crypt abscesses are seen. No granulomata are detected. Basal plasmacytosis is seen with loss of inflammatory gradient. The muscularis mucosa is hypertrophic and is involved by the inflammatory infiltrate.
Case Discussion
This was the first presentation of the patient, acute presentation with gross colonic involvement, mesenteric and hepatic veins thrombosis as a complication. Thromboembolism is rare in inflammatory bowel disease however there is a known increased risk. The patient performed CT pulmonary angiography (unavailable) after this scan that showed no pulmonary embolism. The patient was treated with biological treatment (Infliximab) since then.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.