Presentation
Peritoneal dialysis patient with bloody dialysate fluid.
Patient Data


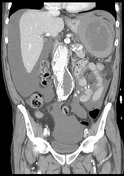

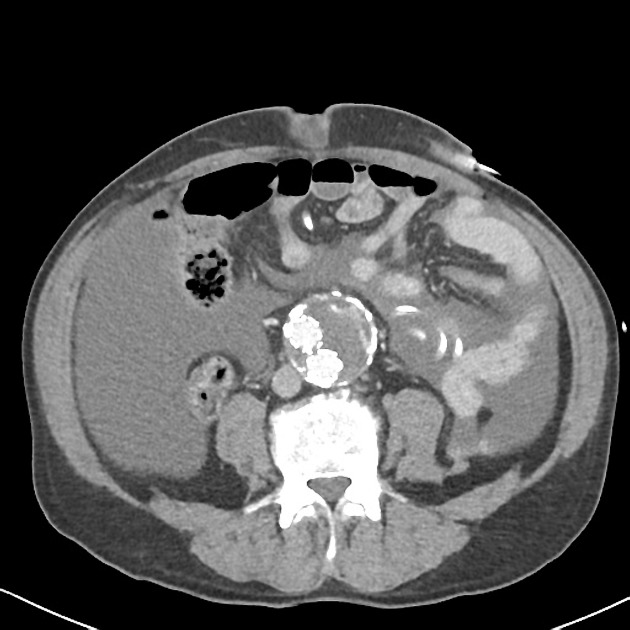
Large splenic subcapsular hematoma with linear superior pole hypodensities. Hematoma extends into the left subphrenic space. Peripheral splenic hyperdensities (shown to be calcification when compared to previous imaging).
Extensive peritoneal free fluid in keeping with peritoneal hemodialysis - this is low density (10-15 HU) with layering or hematocrit effect identified. PD tubing noted.
5.5 cm infrarenal abdominal aneurysm with bi-iliac EVAR stent graft. Atrophic native kidneys with multiple cysts, and atrophic right iliac fossa transplant kidney noted. Irregular liver surface. Adrenal glands, pancreas, gallbladder and bowel is unremarkable.
Case Discussion
This patient had been treated with peritoneal dialysis for a number of years. There was no history of recent or remote trauma, and the patient was essentially asymptomatic aside from bloody peritoneal dialysate and mild abdominal pain.
Atraumatic splenic rupture has been reported as a rare occurrence in both hemodialysis and peritoneal dialysis patients. In a series of 22 dialysis patients who had splenectomy for atraumatic rupture 1, amyloidosis was the most common underlying pathology (~30%), with other underlying pathology including splenomegaly, hemosiderosis, splenic infarcts, and tuberculous granulomas.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.