Presentation
Long-standing non-specific abdominal pain and diarrhea with elevated liver enzymes and jaundice. Positive anti-mitochondria antibody (AMA).
Patient Data







Diffuse increased wall thickness is seen in the colorectal, along with mild pericolic fat stranding, vasa recta engorgement, and several prominent mesenteric lymph nodes, suggesting pan proctocolitis. Additionally, extramural fat deposition leads to the thickening of the perirectal fat and the widening of the presacral space.
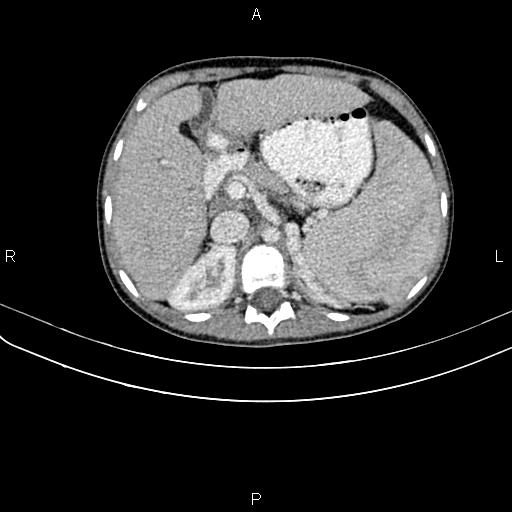
The liver has nodular parenchyma and an irregular margin, and the caudate lobe is enlarged, inferring cirrhosis. Mild periportal hypoattenuation is also observed. A few enlarged lymph nodes are seen in the porta hepatis, with SAD less than 12 mm.
Additionally, dilated collateral vessels are observed in the upper abdomen, particularly in the splenorenal regions, suggesting portal hypertension.
The spleen is markedly enlarged, and its cephalocaudal height measured 210 mm. A 12 mm thin-walled cyst is also noted in the lower pole of the spleen.
Pathology report:
The patient underwent an ultrasound-guided liver biopsy, and histopathology evaluation showed portal and periportal infiltration of lymphocytes, plasmacytes, and eosinophils with scattered fibrosis, which suggests primary biliary cholangitis (PBC).
Case Discussion
This is a known case of ulcerative colitis (UC) associated with primary biliary cholangitis (PBC), which is rare.
Hepatobiliary manifestations are common in inflammatory bowel disease (IBD), affecting 30% of patients with abnormal liver tests and 5% developing chronic liver disease. Up to 90% of UC patients show abnormal liver histology at surgery or autopsy.
The manifestations range from asymptomatic elevated liver function tests to life-threatening conditions and can be caused by:
-
autoimmune background
-
intestinal inflammation
-
metabolic issues
-
drug toxicity
drug-induced liver injury
reactivation of hepatitis B virus
Autoimmune conditions are common in both PBC and UC, suggesting a potential link between these autoimmune diseases, though this relationship requires further clarification. Usually, UC is diagnosed years before PBC. It should be noted that UC associated with PBC tends to be mild, as in this case.
Although it's rare, when investigating abnormal liver function tests in patients with IBD, it's important to consider the coexistence of PBC and IBD. The clinical manifestation, histologic features particularly granulomatous inflammation of the periportal areas, and lab data mainly hyperbilirubinemia and positive AMA (in 95% of cases), help diagnose primary biliary cholangitis (PBC), that previously known as primary biliary cirrhosis.




 Unable to process the form. Check for errors and try again.
Unable to process the form. Check for errors and try again.